The U.S. Food and Drug Administration doesn’t treat every generic drug application the same. Two paths exist: priority review and standard review. The difference isn’t just paperwork-it’s money, timing, and access to life-saving medicines. For companies, getting priority review can mean entering the market two months faster, which translates to hundreds of millions in extra revenue. For patients, it can mean getting affordable drugs sooner, especially when shortages hit.
What’s the difference between priority and standard review?
The FDA’s review clock starts the moment an Abbreviated New Drug Application (ANDA) is officially filed. For standard review, the target completion date is 10 months. For priority review, it’s 8 months. That two-month gap might seem small, but in the generic drug world, it’s everything. Standard review covers most applications-about 70% of all ANDAs submitted. These are drugs with existing generics already on the market, or those that don’t meet special criteria. Priority review is reserved for a select few: first generics (the very first generic version after a brand-name drug’s patent expires), drugs in shortage, or complex generics that offer a meaningful improvement over existing options. The FDA tracks this closely. In 2022, 83.1% of priority review applications met the 8-month goal, compared to 72.3% of standard applications. Why the gap? Priority applications get more attention from reviewers, faster internal routing, and fewer delays in scheduling meetings. But it’s not just about speed-it’s about impact.Who qualifies for priority review?
Not every company can just ask for priority review. The FDA has strict rules. The biggest category is first generics. If you’re the first to file a complete ANDA after a brand-name drug’s patent or exclusivity ends, you automatically qualify. These drugs often come with 180 days of market exclusivity, meaning no other generic can enter during that time. That’s why companies race to be first. The second major category is drugs in shortage. The FDA defines a shortage as a situation where the supply of a drug can’t meet patient demand, and it’s serious enough to affect health outcomes. In 2022, nearly 40% of priority review applications were for drugs on the official shortage list-things like antibiotics, chemotherapy agents, or injectables used in hospitals. There’s also a third path: complex generics that are medically important. These aren’t just harder to make-they’re harder to copy. Think inhalers, topical creams, or long-acting injectables. If your version is safer, more effective, or easier to use than what’s already out there, the FDA may grant priority status.The new U.S. manufacturing pilot program
In October 2023, the FDA launched a game-changing addition to the priority review system: the ANDA Prioritization Pilot Program. This isn’t just about speed anymore-it’s about supply chain security. To qualify, a generic drug application must meet three strict criteria:- Bioequivalence testing done in the United States
- Finished dosage form manufactured in the U.S.
- Active pharmaceutical ingredient (API) sourced entirely from U.S.-based suppliers

Why does this matter for patients and the healthcare system?
Generic drugs make up 88.6% of all prescriptions filled in the U.S., but they cost only 15.3% of what brand-name drugs do. In 2022, they saved the system $370 billion. But savings only happen if those drugs are available. Priority review gets drugs to market faster. For a first generic, that two-month head start can mean $200-500 million in extra revenue. That’s why companies fight to be first. But it’s not just about profits. When a drug is in shortage-say, a common antibiotic or insulin-the FDA fast-tracks approval to prevent harm. Patients waiting weeks or months for a critical drug don’t care about corporate profits. They just need access. The U.S. manufacturing pilot adds another layer. If more generic drugs are made here, supply chains become more resilient. The FDA aims to raise the share of U.S.-manufactured generics from 28% to 40% within five years. That’s not just good for national security-it’s good for consistent availability.What’s holding companies back?
Even with the incentives, many generic manufacturers struggle. The biggest hurdle? Complexity. Nearly one-third of ANDAs get a Complete Response Letter (CRL) in the first round, usually because of issues with chemistry, manufacturing, or controls (CMC). On average, an ANDA needs 1.7 review cycles to get approved. Each cycle adds about four months to the timeline. That’s why more companies are using the FDA’s pre-submission meetings. In 2020, only 41% of sponsors met with the FDA before filing. By 2023, that number jumped to 63%. These early discussions help companies fix problems before they submit, improving first-cycle approval rates from 24.1% to 38.7%. The FDA also launched a Complex Generic Drug Product Pilot Program in early 2023 to help with harder-to-copy products like inhalers and topical gels. These make up 18.3% of pending applications but only 9.7% of approvals. With more guidance, that gap is starting to close.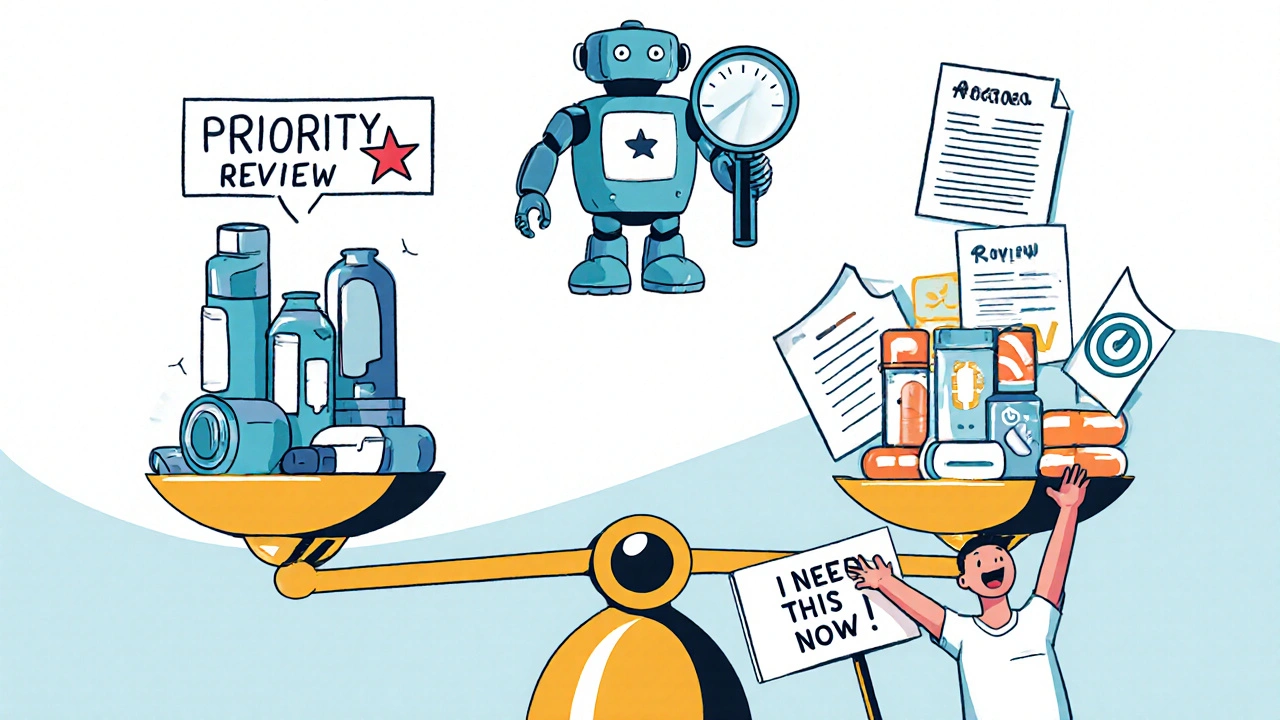
What’s next for FDA generic reviews?
The FDA is testing AI tools to speed up reviews. In internal trials, AI reduced review times for simple applications by nearly 19%. By late 2024, these tools could be rolled out to handle routine checks-like verifying labeling consistency or checking for duplicate patents. Industry analysts predict that by 2026, these changes could cut the average time from patent expiry to generic approval from 2.7 years to around 2.3 years. That’s 4.3 months faster. If realized, that could save the U.S. healthcare system an extra $18.7 billion a year. The future isn’t just about faster approvals-it’s about smarter ones. The FDA is moving from a reactive system to a proactive one. Priority review isn’t just a reward anymore. It’s a tool to shape the market, ensure supply, and protect public health.How do you know if your drug qualifies?
If you’re a generic manufacturer, ask yourself:- Is this the first generic for this brand-name drug? If yes, you likely qualify for priority review.
- Is this drug on the FDA’s shortage list? If yes, you’re eligible.
- Are you manufacturing the finished product and sourcing your API in the U.S.? If yes, you can apply for the pilot program.
- Is this a complex product like an inhaler or injectable? If yes, consider the Complex Generic Pilot for early feedback.
What’s the difference between priority review and standard review for generic drugs?
Priority review takes 8 months from submission, while standard review takes 10 months. Priority review is reserved for first generics, drugs in shortage, or complex generics that offer a medical advantage. Standard review applies to all other generic applications.
Can any company request priority review?
No. Priority review is not something you can ask for arbitrarily. The FDA grants it only if the application meets specific criteria: being the first generic after patent expiry, addressing a drug shortage, or being a medically important complex product. The agency evaluates each application against these rules.
What is the ANDA Prioritization Pilot Program?
Launched in October 2023, this program gives priority review status to ANDAs that conduct bioequivalence testing in the U.S., manufacture the finished drug in the U.S., and use U.S.-sourced active ingredients. It’s designed to strengthen domestic supply chains and reduce reliance on foreign manufacturing.
Why are so many generic applications rejected on the first try?
About 31.7% of ANDAs receive a Complete Response Letter (CRL) in the first review cycle. The most common reason is chemistry, manufacturing, and controls (CMC) issues-like inconsistent drug formulation, unclear testing methods, or packaging problems. Many companies now use pre-submission meetings with the FDA to fix these before filing.
How does the FDA decide which drugs are in shortage?
The FDA defines a shortage as a situation where the total supply of a drug is insufficient to meet patient demand, and the shortage poses a risk to public health. Manufacturers must report potential shortages to the FDA, and the agency evaluates clinical impact, availability of alternatives, and patient safety before listing a drug as officially in shortage.
Is the U.S. manufacturing requirement realistic for all generic drugs?
For simple pills, yes. But for complex products like inhalers or injectables, many specialized ingredients still come from Europe or Asia. Only 12.3% of current applicants meet all three U.S. criteria. The FDA acknowledges this and is working with industry to build domestic capacity for critical materials over the next five years.





One comment
Man, I didn’t realize how much of a race it is just to get a generic on the shelf. That 180-day exclusivity window? That’s where the real money’s at. Companies are basically betting their entire Q3 on being first to file. And yeah, it’s brutal for patients waiting on insulin or antibiotics-but if you’re the one who cracked it, you’re basically printing money for two months straight.
It is deeply concerning that the regulatory framework has become so entangled with corporate profit motives that the health of the American public is now contingent upon the speed at which a pharmaceutical entity can navigate bureaucratic channels. The FDA, in its current configuration, functions less as a guardian of public health and more as an arbiter of market advantage.
Interesting. In India, we make most of the APIs, but we rarely get priority review because the FDA doesn't trust our manufacturing standards. But if you make the same drug in the U.S. with the same API, suddenly it's 'secure supply chain.' The irony is thick. I wonder how many U.S.-made generics are actually better-or just more expensive.
so like… if you make a pill in the usa and the chem stuff is also from usa, you get to skip the line? that’s wild. but like… 12% of companies can even do that? who’s gonna make the cheap generics then? also i think i saw a typo in the article lol
The emphasis on domestic manufacturing is a necessary step toward long-term pharmaceutical sovereignty. However, it must be implemented with equitable support for small manufacturers who lack the capital to retool facilities. Without targeted incentives, this policy risks consolidating market power among a few large players, ultimately undermining the very affordability that generics are meant to ensure.
Just wanted to say-this is one of the clearest breakdowns I’ve seen on how the FDA actually works behind the scenes. Most people think generics are just ‘copycat drugs,’ but the complexity involved, especially with inhalers and injectables, is insane. And the fact that they’re using AI to check labeling? That’s next level. 👍
AI cutting review time by 19%? That’s huge. Imagine if they used it to auto-flag duplicate patents or mismatched batch numbers-no more human error on the small stuff. Also, big props to the FDA for actually listening to industry feedback on pre-submission meetings. 63% using them now? That’s a win for everyone. 🤖💊
so the whole ‘make it in america’ thing is just a fancy way to make generics more expensive? like… i get the supply chain thing, but if i’m diabetic and my insulin generic just got delayed because the API had to come from ohio instead of hyderabad… is that really better?
It’s fascinating how the FDA’s criteria for priority review have evolved from pure medical urgency to include economic and geopolitical factors. The pilot program isn’t just about speed-it’s about reshaping global pharma trade. But I wonder: will this actually reduce shortages, or just shift them to other countries that can’t compete? The data on U.S. API capacity growth is promising, but it’s still a drop in the ocean.
Make drugs in America. Screw India. We’re #1. 🇺🇸
One thing everyone’s missing: the pre-submission meetings are the real game-changer. Companies that used to submit half-baked applications just to ‘get in the door’ are now investing months in preparation. That’s not just efficiency-it’s quality. The jump from 24% to 38% first-cycle approval rates proves it. The FDA didn’t just change the rules; they raised the bar-and the industry rose to meet it.