Rheumatoid arthritis isn’t just stiff joints or old-age aches. It’s your own immune system turning against you-attacking the lining of your joints, causing swelling, pain, and eventually, permanent damage. Unlike osteoarthritis, which comes from wear and tear, rheumatoid arthritis (RA) is an autoimmune disease. That means your body’s defense system, designed to fight infections, starts mistaking healthy tissue for a threat. And it doesn’t stop at the joints. RA can affect your lungs, heart, eyes, and even your blood vessels.
How Rheumatoid Arthritis Actually Starts
No one knows exactly what flips the switch that turns RA on. But we do know the pieces. Genetics play a role-certain versions of HLA genes make some people more likely to develop it. Environmental triggers like smoking, viral infections, or even long-term exposure to silica dust can push those at risk over the edge. Women are two to three times more likely to get RA than men, and it usually shows up between ages 30 and 60, though it can strike at any age.
The real damage happens in the synovium-the thin membrane that lines your joints and makes fluid to keep them moving smoothly. When your immune system attacks it, the synovium swells, becomes inflamed, and starts eating away at cartilage and bone. That’s why RA causes not just pain, but deformities over time. The most common early signs? Swollen, tender fingers and toes, especially in the morning. That stiffness can last longer than an hour-sometimes two or three. It’s not just discomfort. It’s a signal your body is under siege.
What Makes RA Different From Other Arthritis
Osteoarthritis is about broken-down cartilage. RA is about an out-of-control immune system. That’s why the symptoms don’t match. With RA, you get symmetry-both wrists, both knees, both ankles. With osteoarthritis, it’s usually one side. RA also brings systemic symptoms: fatigue, low-grade fever, weight loss. You might develop rheumatoid nodules-hard lumps under the skin near elbows or fingers. Some people even get dry eyes and mouth, a sign of Sjögren’s syndrome, which often comes with RA.
Doctors diagnose RA using a mix of blood tests, imaging, and physical exams. The key markers are rheumatoid factor (RF) and anti-CCP antibodies. If both are positive, it’s a strong clue. X-rays and MRIs show early signs like soft tissue swelling, then bone thinning, and finally, erosions where the joint is literally being eaten away. The longer RA goes untreated, the more damage piles up. That’s why timing matters more than almost anything else.
Why Early Treatment Changes Everything
There’s a window-about three to six months after symptoms start-where aggressive treatment can stop joint damage before it’s permanent. After that, the damage is often irreversible. That’s why experts say: treat fast, treat hard. The goal isn’t just to feel better. It’s to reach remission-where inflammation drops so low, symptoms vanish, and your joints are protected.
First-line treatment is almost always methotrexate. It’s cheap, effective, and has been the backbone of RA care for decades. But for many, it’s not enough. That’s where biologics come in.
What Are Biologic Therapies?
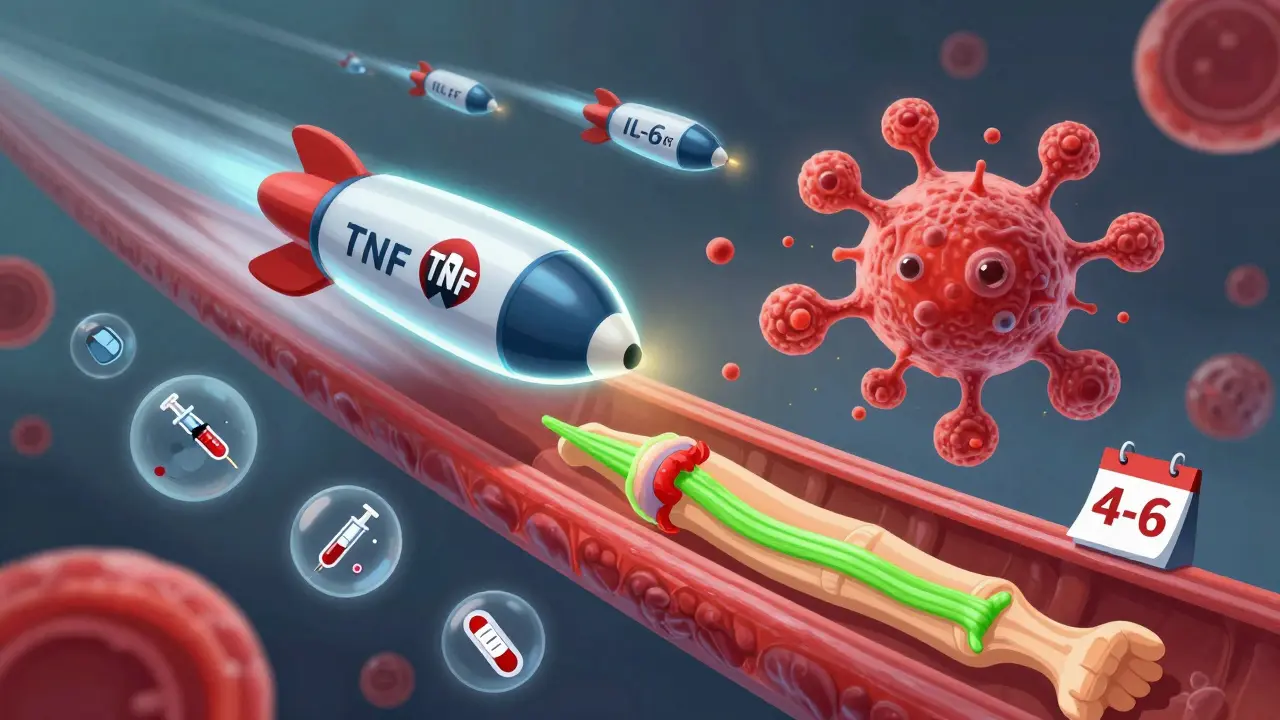
Biologics are a type of disease-modifying drug made from living cells. They don’t just calm inflammation-they target specific parts of the immune system that drive RA. Think of them as precision missiles instead of shotgun blasts.
There are four main types:
- TNF inhibitors (like adalimumab, etanercept, infliximab): Block tumor necrosis factor, a major inflammation trigger. These were the first biologics approved and still make up over half of all biologic prescriptions.
- IL-6 inhibitors (like tocilizumab): Interrupt interleukin-6, a protein that fuels joint destruction and fatigue.
- B-cell inhibitors (like rituximab): Deplete B-cells, the immune cells that produce harmful antibodies in RA.
- T-cell costimulation blockers (like abatacept): Stop T-cells from activating and attacking joint tissue.
Most biologics are given by injection or IV, usually once every few weeks. They’re not magic pills. But when they work, they work hard. Clinical trials show that when paired with methotrexate, biologics reduce disease activity by 50% or more in about 60% of patients. That means less pain, less swelling, and the ability to move again.
The Real Cost-Money, Side Effects, and Life
Biologics are expensive. Annual costs range from $15,000 to $60,000. Even with insurance, copays can hit $500 a month. That’s why nearly half of patients say cost is a barrier to sticking with treatment. Some stop because they can’t afford it. Others stop because of side effects.
Biologics weaken your immune system’s ability to fight infections. You’re at higher risk for pneumonia, tuberculosis, and skin infections. That’s why doctors test for TB before starting treatment. Some patients get serious infections. A few develop lymphoma, though the absolute risk is still low.
On Reddit, users talk about injection site reactions-redness, itching, burning. One person said, “I’ve had to switch biologics three times because my skin just hates them.” Another said, “After starting tocilizumab, I played piano again for the first time in five years.”
It’s not just physical. Living with RA is exhausting. The mental toll of chronic pain, unpredictability of flares, and constant medical appointments weighs heavy. That’s why support networks like the Arthritis Foundation’s Live Yes! Network matter. They offer tools, peer groups, and education that help people manage not just the disease, but their lives with it.
What’s New in RA Treatment
The landscape is changing fast. In 2023, the FDA approved the first biosimilar to adalimumab (adalimumab-adaz). Biosimilars are nearly identical to brand-name biologics but cost 15-20% less. That’s a big deal for patients and insurers.
In early 2024, upadacitinib (Rinvoq) got approval for early RA. It’s a JAK inhibitor-a newer class of drugs that work inside cells, not just on the surface. JAK inhibitors are taken as pills, which some patients prefer over injections.
Researchers are also hunting for biomarkers. A 2023 study in Nature Medicine used genetic markers to predict who would respond to methotrexate with 85% accuracy. That could mean fewer trial-and-error switches. In the next few years, new drugs like TYK2 inhibitors (deucravacitinib) could offer more options with fewer side effects.

How to Manage RA Beyond Medication
Medicine alone isn’t enough. Exercise helps. Just 150 minutes a week of walking, swimming, or cycling reduces pain and stiffness. Losing 5-10% of your body weight can cut disease activity by 20-30%. That’s not a side effect-it’s a treatment.
Physical therapy keeps joints mobile. Occupational therapy teaches you how to protect your hands and wrists during daily tasks. Apps like MyRA help track symptoms, meds, and flares. The CDC’s self-management workshops have been shown to reduce pain by 20% in just six months.
And don’t ignore mental health. Depression and anxiety are common in RA. Talking to a counselor, joining a support group, or even just connecting with others who get it can make a real difference.
What to Expect If You Start Biologics
It’s not instant. You might not feel better for weeks. Some people notice improvement after 4-6 weeks. Others take 3-6 months. Your doctor will check your disease activity every 3-6 months using blood tests and joint exams. If you’re not reaching your target-remission or low disease activity-you’ll adjust the treatment.
You’ll need regular blood work to watch for liver issues or low blood counts. You’ll get screened for infections. You’ll be told to avoid live vaccines. And you’ll need to tell every doctor you see-dentist, surgeon, ER-that you’re on a biologic. That’s not optional. It’s life-saving.
Many people worry about long-term safety. The truth? We’ve been using biologics for over 25 years. The risks are real, but they’re manageable. For most, the benefit of keeping their joints, their mobility, and their independence outweighs the risks.
Final Thoughts: It’s Not a Death Sentence
Rheumatoid arthritis is serious. But it’s not a sentence to a life of pain and disability. With early diagnosis, the right combination of meds, lifestyle changes, and support, most people can live full, active lives. The goal isn’t to cure it. It’s to control it-so it doesn’t control you.
If you’re newly diagnosed, don’t wait. Don’t accept stiffness as normal. Push for a rheumatologist. Ask about biologics if methotrexate isn’t enough. Talk to others who’ve been there. And remember: science has come a long way. What was once a slow decline is now a manageable condition-with real hope for a better future.
Can rheumatoid arthritis be cured?
No, there is no cure for rheumatoid arthritis yet. But with early and aggressive treatment, many people can achieve remission-where symptoms disappear and joint damage stops progressing. The goal is to control the disease so it doesn’t limit your life.
How long does it take for biologics to work?
Most people start noticing improvements in 4 to 6 weeks, but full benefits can take 3 to 6 months. Patience is key. If you don’t feel better after 3 months, talk to your doctor about adjusting your treatment. Not all biologics work for everyone, and switching is common.
Are biologics safe for long-term use?
Biologics have been used for over 25 years, and their long-term safety profile is well-studied. The main risks are increased infections and a slightly higher chance of certain cancers, like lymphoma. But for most patients, the benefits-preserving joints, reducing pain, regaining function-outweigh the risks. Regular monitoring helps catch problems early.
Can I stop taking biologics if I feel better?
Never stop biologics without talking to your rheumatologist. Stopping can cause your disease to flare back, sometimes worse than before. Even in remission, most people need to stay on some form of treatment to keep the disease suppressed. Some may be able to reduce dosage under close supervision, but stopping entirely is rarely advised.
What if I can’t afford biologics?
Many pharmaceutical companies offer patient assistance programs that can lower or eliminate out-of-pocket costs. Biosimilars-cheaper versions of brand-name biologics-are now available and covered by most insurers. Talk to your doctor, pharmacist, or a patient advocate at the Arthritis Foundation. You’re not alone, and help is available.
Do biologics cause weight gain?
Biologics themselves don’t directly cause weight gain. But some people gain weight after starting treatment because they feel better and become more active-or because they reduce steroid use, which can cause fluid retention. Weight gain is more often linked to reduced activity before treatment or other medications like prednisone. Maintaining a healthy diet and regular exercise helps manage weight regardless of your treatment.





One comment
I started biologics last year and honestly? My hands don't ache in the morning anymore. I can hold my coffee cup without wincing. That's not a minor thing.
So many people think RA is just 'bad arthritis'-it's not. It's a full-body autoimmune war. And yes, biologics are expensive, but if you're not getting help from methotrexate, you owe it to yourself to push for a referral. Your joints won't wait.
IF YOU HAVE RA AND YOU'RE NOT MOVING-YOU'RE LOSING. I started swimming three times a week after my third biologic switch-and I cried the first time I reached overhead without pain. It's not just medicine. It's movement. It's life.
Biologics don't work for everyone. I tried three. Got zero relief. Still in pain. So don't act like it's a miracle cure. It's a gamble with a $50k price tag.
Early diagnosis is critical. I was misdiagnosed for two years because my doctor thought I was just tired. By the time I saw a rheumatologist, I had early joint erosion. Don't wait. Get anti-CCP tested. It's more specific than RF. And push for an MRI if symptoms persist.
The psychological burden of RA is understated. Chronic pain alters neural pathways. Depression isn't a reaction-it's a neurological consequence. Support groups aren't optional; they're part of the treatment protocol.
Regarding JAK inhibitors: while oral administration is convenient, the FDA black box warning for thrombosis and malignancy remains a concern. Biologics still hold a superior long-term safety profile in meta-analyses. The choice should be individualized based on comorbidities and risk stratification.