When you prescribe a generic medication, you’re not just choosing a cheaper option-you’re stepping into a legal gray zone that’s gotten riskier over the last decade. The Supreme Court didn’t just change drug pricing rules; it shifted the entire weight of responsibility onto your shoulders. If a patient suffers harm from a generic drug, the manufacturer can’t be sued. That means physician liability is now the main target in lawsuits that once went after pharmaceutical companies.
Why Generic Drugs Changed Everything
In 2011 and 2013, the U.S. Supreme Court made two rulings-PLIVA v. Mensing and Mutual Pharmaceutical v. Bartlett-that changed how liability works for generic drugs. These cases involved patients who were severely injured by generic versions of medications. One woman, Karen Bartlett, lost 65% of her skin after taking a generic anti-inflammatory. She sued the manufacturer. The Court said no: generic drugmakers can’t be held liable for inadequate warnings because federal law forces them to copy the brand-name label exactly. They can’t update it, even if new dangers emerge. That left patients with nowhere to turn. So they started suing the doctors who prescribed the drugs.The Three Legal Elements You Can’t Ignore
To win a malpractice case against you, a plaintiff must prove three things:- Duty: You had a doctor-patient relationship. That’s easy to prove.
- Dereliction: You didn’t meet the standard of care. Did you warn the patient about known side effects? Did you know the drug had a narrow therapeutic index? Did you ignore warnings from the FDA or medical literature?
- Direct cause: The medication directly caused the injury. This is where things get messy. Was it the drug? The substitution? The patient’s other meds? Your documentation will be the deciding factor.
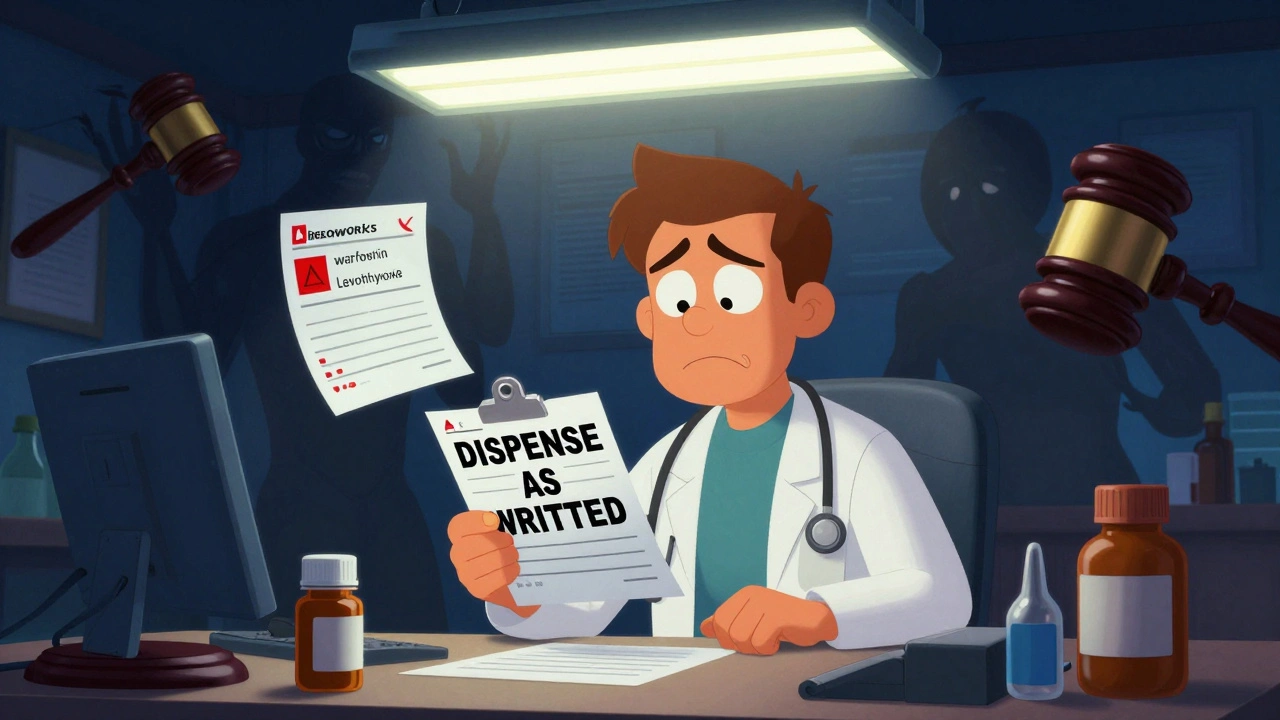
Take the case of a patient on warfarin. If you prescribe it and don’t specify ‘dispense as written,’ the pharmacist swaps it for a generic. The generic has slightly different fillers. The patient’s INR spikes. They bleed internally. You’re now on the hook-not because you made a clinical error, but because you didn’t protect yourself legally.
State Laws Vary-And So Do Your Risks
Forty-nine states let pharmacists substitute generics unless you write ‘do not substitute’ or ‘dispense as written.’ But here’s the catch: 17 states don’t require pharmacists to tell you when they make the switch. That means you could be prescribing a brand-name drug, and the patient walks out with a generic you never approved. In Illinois, courts have ruled that generic manufacturers still have a duty to update labels if a drug is dangerously flawed. But in most states, including Alabama and Texas, the federal preemption doctrine holds firm. That means your liability depends entirely on where you practice-and where your patient lives.
What You’re Doing Now Might Be Making Things Worse
A 2022 survey of 1,200 physicians found that 68% feel more anxious prescribing generics. Forty-two percent admit they sometimes prescribe the more expensive brand-name drug-not because it’s better clinically, but because they’re scared of being sued. That’s not just expensive for patients. It’s a sign the system is broken. One doctor in Massachusetts now spends 15 to 20 extra minutes per visit writing out detailed warnings: ‘Do not drive while taking this. Risk of dizziness. May cause liver damage. Do not combine with alcohol.’ He’s not doing it because it’s good medicine. He’s doing it because his malpractice insurer told him to-or risk a premium hike.Documentation Is Your Only Shield
The difference between a lawsuit that settles and one that destroys your career? Paperwork. A 2023 report from Medical Risk Management found that physicians who document specific, personalized counseling about generic substitution reduce their liability exposure by 58%. Generic notes like ‘medication discussed’? Useless. Courts see that as negligence. Here’s what works:- Write: ‘I discussed potential side effects of [generic name], including [specific risk], and advised patient to avoid [specific activity].’
- Use ‘dispense as written’ for drugs with narrow therapeutic windows: warfarin, levothyroxine, phenytoin, lithium, cyclosporine.
- Record the patient’s understanding: ‘Patient stated they understand risks and will call if they develop rash, dizziness, or jaundice.’
Electronic health records now have mandatory fields for this. Epic Systems added them in 2021. If you skip it, your system flags it. That’s not a glitch-it’s a legal safeguard.
Insurance Is Getting More Expensive
Your malpractice premiums are rising. Not because you’re making more mistakes-but because the risk profile has changed. According to the American Professional Agency, physicians who routinely authorize generic substitutions without documented counseling pay an average 7.3% higher premium. That’s $1,200 to $2,500 extra per year for a primary care doctor. Between 2013 and 2022, premiums for primary care physicians rose 22.7%. The Medical Liability Monitor says generic drug lawsuits are a major driver.
The Bigger Picture: A System in Crisis
Generic drugs make up 90% of all prescriptions filled in the U.S. That’s good for costs-but bad for accountability. The system was designed to save money, not to protect patients or doctors. Congress has tried to fix it. H.R. 958, the ‘Preserving Access to Prescription Medications Act,’ would have restored some liability to manufacturers. It died in committee in 2021. Pharmaceutical companies spent $14.7 million lobbying against it since 2011. Meanwhile, 18 states introduced bills in 2023 requiring pharmacists to notify physicians within 24 hours of substituting a generic for high-risk drugs. None have passed yet.What You Can Do Today
You can’t control what the FDA allows or what the courts decide. But you can control your practice.- Always ask: ‘Is this drug on the narrow therapeutic index list?’ If yes, write ‘dispense as written.’
- Never assume the patient knows the risks. Even if they’ve taken it before-generics change.
- Document every conversation. Use exact language. Don’t rely on templates.
- Know your state’s substitution laws. If your state doesn’t require notification, assume the substitution happened without your knowledge.
- Review your malpractice policy. Does it cover generic-related claims? If not, ask your insurer.
There’s no perfect solution. But if you treat documentation like a legal contract-not just a bureaucratic chore-you’ll protect yourself, your patients, and your career.
What’s Next?
Legal scholars predict a 45% rise in physician-targeted lawsuits involving generic drugs by 2027. The Supreme Court has declined to revisit the Mensing/Bartlett rulings. That means the status quo stays. You’re not alone in this. But you can’t afford to wait for someone else to fix it.Can I be sued if a patient is harmed by a generic drug I prescribed?
Yes. Since the 2011 and 2013 Supreme Court rulings, generic drug manufacturers are generally immune from liability. Patients who are harmed often sue the prescribing physician instead, especially if there’s no clear documentation that side effects were discussed or if the drug had a narrow therapeutic index.
What’s the difference between ‘dispense as written’ and ‘do not substitute’?
They mean the same thing legally. Both prevent the pharmacist from substituting a generic for a brand-name drug. ‘Dispense as written’ is the more commonly used term on prescriptions. Always use it for high-risk medications like warfarin, levothyroxine, or seizure drugs.
Do I need to document counseling for every generic prescription?
For high-risk drugs, yes. For routine medications like antibiotics or statins, documentation is still strongly recommended. Courts look for evidence you assessed risk. A generic note like ‘medication discussed’ won’t hold up. Use specific language: ‘I explained the risk of dizziness and advised avoiding driving.’
Why can’t generic manufacturers update their warning labels?
Federal law requires generic drugs to have the same label as the brand-name version. Manufacturers can’t change warnings unless the brand-name company updates its label first and the FDA approves the change. This legal requirement is what led to the Supreme Court’s preemption rulings.
Are there any states where physicians have less liability for generics?
Illinois is an exception. In one case, the state court ruled that generic manufacturers must update labels if a drug is inherently dangerous-even if the brand-name label hasn’t changed. This creates a small window of liability for manufacturers, which reduces pressure on physicians. But in 48 other states, federal preemption rules apply.
How can I reduce my insurance premiums related to generic prescribing?
Document specific patient counseling for every generic prescription, especially for high-risk drugs. Use exact phrases like ‘I advised patient to avoid driving due to dizziness risk.’ Avoid vague notes. Insurers reward detailed documentation with lower premiums-some offer up to 10% discounts for verified compliance.




One comment
Bro, I just prescribed a generic statin and my patient had a rash. Now I’m terrified to write anything that isn’t a legal brief. This system is rigged.
I’ve been doing this for 18 years and I’ve never once had a lawsuit. But I document everything like my license depends on it - because it does. I write: 'Discussed risk of dizziness with patient, confirmed understanding, advised against driving.' No fluff. No templates. Just facts. If you’re not doing this, you’re playing Russian roulette with your career.
I’ve seen residents get crushed because they wrote 'medication discussed.' Courts see that as negligence. It’s not about being paranoid - it’s about being smart.
And yes, it takes time. But you know what takes more time? Court dates, depositions, and watching your reputation burn while your insurer dithers.
My clinic now has a checklist for high-risk generics. Warfarin, levothyroxine, lithium - if it’s on the list, you get the full spiel and a signature. It’s not ideal, but it’s the new standard.
Also, stop assuming patients know what ‘narrow therapeutic index’ means. They don’t. Explain it like they’re 12. 'This medicine is like a tightrope - too little does nothing, too much can kill you.' That’s the kind of language that sticks - and that courts respect.
Ugh I’m so sick of this. My malpractice premium went up 18% last year and I swear it’s because of these damn generics. I’m literally paying more to avoid getting sued for something I didn’t even control.
And don’t even get me started on pharmacists - they swap stuff without telling me and then I’m the one who gets blamed. I had a patient show up with a different generic and I had no idea until she came in with liver enzymes through the roof.
Why isn’t anyone holding the FDA accountable? This is a disaster waiting to happen to every single doctor in America.
Y’all are losing your minds. This is just Big Pharma’s way of offloading risk onto us so they can keep making billions. The Supreme Court? Totally bought and paid for. You think they really care about patients? Nah. They care about profits. And now we’re the cannon fodder.
I saw a guy on Reddit who got a generic version of his seizure med and had a seizure in front of his kid. The manufacturer? Immune. The pharmacist? Not liable. The doctor? Sued for $3M. This isn’t medicine - it’s a lawsuit lottery.
And don’t tell me to document more. I’ve got 25 patients a day. I don’t have time to write essays. My EHR auto-fills ‘medication discussed’ and I’m supposed to be grateful? That’s not documentation - that’s a joke.
Someone needs to start a movement. #SueThePharmaNotTheDoc
This isn’t about documentation it’s about systemic corruption and the complete erosion of accountability in healthcare. The fact that a drug manufacturer can knowingly sell a product that causes severe harm and walk away without consequence while the physician who merely prescribed it gets sued is a moral outrage. The FDA is complicit. The courts are complicit. The insurance companies are complicit. And you people are just adjusting your note templates like it’s a minor inconvenience. Wake up. This is the tip of the iceberg. Next it’ll be nurses being sued for administering meds. Then coders for coding wrong. Then janitors for cleaning the floor where the patient slipped. This is how authoritarian systems collapse - by making the frontline workers pay for the sins of the powerful. And you’re all too busy filling out checkboxes to notice.
Hey, I get it - this is terrifying. But you’re not alone. I used to dread prescribing generics too. Then I started talking to my patients like humans, not cases. I say: 'I know this isn’t the brand you’re used to. Let me explain why I think this one’s safe for you - and what to watch out for.'
Most patients are grateful. They don’t want to get hurt. They just want to understand. And when you take five extra minutes to actually listen, they’ll tell you things you’d never catch in a chart.
My trick? I use the EHR’s new mandatory fields. I don’t fight them - I lean into them. It forces me to slow down. And guess what? My premiums went down 8% last year. Not because I’m perfect - but because I’m transparent.
Also - if you’re scared, ask your insurer what they want to see. Most will give you a checklist. Use it. It’s not busywork. It’s armor.
We’re not powerless here. We just have to change how we show up.
I’ve been doing this since 2008 and I’ve never had a problem. Just write what you actually said. Not what you think sounds good. Just the truth. Patient asked about side effects I told them dizziness and liver issues and they nodded. That’s it. That’s all you need.
Oh wow. So you’re telling me that after spending 10 years in med school, 3 years in residency, and another 5 years building a practice, the thing that’s going to destroy me isn’t a misdiagnosis or a missed cancer - it’s a pharmacist swapping a pill I didn’t even know was swapped? And now I have to become a lawyer to prescribe Tylenol? This isn’t medicine anymore. It’s a trap. And the worst part? The patients who need generics the most - the ones on Medicaid, the elderly, the poor - they’re the ones getting screwed the hardest because we’re all too scared to prescribe them. So now they’re paying more or going without. Brilliant.
Wait so if I write 'dispense as written' does that mean I have to pay more for the brand name? Because if so I’m not doing it. My patients can’t afford it. I’m not going to make them choose between rent and their meds just because the system is broken. Someone else can fix this. Not me.
My friend, this is not merely a legal issue - it is a metaphysical crisis of modernity. We have outsourced our humanity to algorithms, to insurance forms, to FDA mandates, and now we are being punished for the soulless efficiency of a system that never cared for us in the first place. The generic pill is a symbol: a hollow vessel of capitalism’s indifference. When the body fails, who do we blame? The doctor? The pharmacist? The chemist who mixed the powder? Or the invisible hand that demanded cheaper, faster, and colder? We are not healers anymore. We are clerks in a temple of profit. And the gods have already left.
But - here is the paradox - in documenting every breath, every word, every sigh - we reclaim our dignity. Not as lawyers. Not as targets. But as witnesses. And perhaps, in this act of witnessing, we become human again.
Look I’ve been in this game since 2005 and I’ve seen every trend come and go. This one’s real. The lawsuits are climbing. The premiums are climbing. The silence from Congress is deafening. And the worst part? The people who need generics the most - low income, elderly, rural - they’re the ones getting caught in the crossfire because we’re too scared to prescribe them properly. You think I want to spend 20 minutes per visit reading off a script? No. But I do it because if I don’t, I’m not just risking my license - I’m risking my life’s work. And if you think you’re safe because you’ve never been sued? You’re just lucky. Luck doesn’t last. Documentation does.
I’ve had patients come back months later saying they didn’t even know they were on a generic. That’s on me. Not the pharmacist. Not the manufacturer. Me. And now I make sure they know. I say it out loud. I write it down. I make them repeat it back. It’s exhausting. But it’s the only thing keeping me out of court.
And if your EHR doesn’t force you to do it? Change systems. Or change jobs. Because the system isn’t broken - it’s rigged. And if you’re not fighting it, you’re part of it.