When a pharmaceutical company makes even a small change to how a drug is made - like swapping out a machine, moving a step to a different room, or tweaking the temperature in a mixing tank - it’s not just an internal decision. It’s a regulatory event. And if you get it wrong, the FDA can shut down your product, issue a warning letter, or force a recall. This isn’t theoretical. In 2023, manufacturing changes were behind 22% of all FDA warning letters issued that year. Most of those came from companies that misclassified a change as minor when it was actually major.
Why Do Manufacturing Changes Need Approval?
Every drug on the market has a regulatory file. That file includes every detail about how it’s made: the ingredients, the equipment, the process steps, the testing methods. When you first get approval, the FDA says, "This is how you make it, and this is what it must look like." If you change anything after that, you’re changing the product - even if you think it’s the same. The goal isn’t to slow you down. It’s to make sure the medicine you take today works the same way it did last month. A change in the mixer’s speed might alter how the active ingredient dissolves. A new supplier for a container might let in moisture. A different cleaning protocol could leave behind residues. These aren’t small risks. They’re patient safety risks.The Three Tiers: What’s Major, Moderate, and Minor?
The FDA uses a simple but strict system: three categories for reporting changes. You don’t pick which one - the risk does.- Major changes need Prior Approval Supplement (PAS). You can’t make the change until the FDA says yes. This includes switching the way you make the active ingredient, moving production to a new country, or changing equipment that affects how the drug behaves in the body. For example, replacing a lyophilizer (freeze-dryer) with a different model? That’s PAS. No exceptions.
- Moderate changes use CBE-30. You can make the change, but you must tell the FDA at least 30 days before you start shipping the new version. This covers things like replacing a pump with an identical model from the same manufacturer, or updating software on a filling machine that doesn’t change the process. You still need data to prove it won’t hurt quality - but you don’t need to wait for approval.
- Minor changes go in your annual report. These are tiny adjustments: moving a non-critical step to another clean room in the same building, changing the label font size, or updating a calibration schedule. You don’t notify the FDA ahead of time. You just log it and report it once a year.
What Happens If You Get It Wrong?
In 2023, the FDA issued four warning letters specifically for companies that classified a major equipment change as moderate or minor. One case involved Lupin Pharmaceuticals replacing a critical freeze-dryer without submitting a PAS. The product was already on the shelf. The FDA didn’t just ask for a correction - they demanded a full recall. Misclassification isn’t always a mistake. Sometimes it’s a cost-cutting move. A company might think, "Our change is similar to last year’s - we’ll just file it as CBE-30." But if the new equipment has a different material of construction, or a different cleaning cycle, it’s not equivalent. The FDA’s 2022 guidance says "equivalent" means: same principle of operation, same critical dimensions, same material. If any of those differ, it’s not equivalent. And if it’s not equivalent, it’s PAS.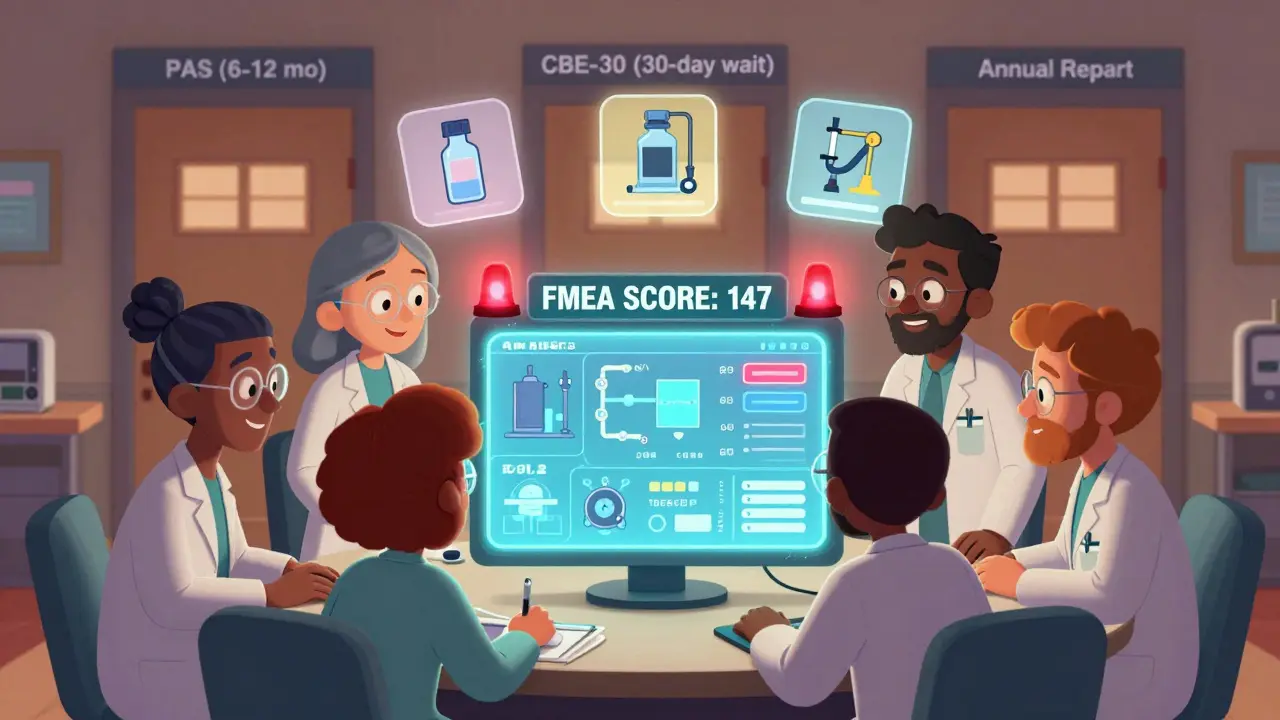
How Do You Know Which Category to Use?
There’s no checklist that covers every scenario. But there’s a process. Start with risk. Ask: "Could this change affect the drug’s identity, strength, purity, or potency?" If yes, it’s not minor. Then look at the data. Do you have stability studies? Batch-to-batch comparisons? Validation reports? If you don’t, you’re guessing - and the FDA will call that out. The FDA’s 2021 guidance for biologics includes a table of common changes and their recommended categories. Even if you’re making small-molecule drugs, it’s a useful reference. For example:- Replacing a filter with one of the same pore size and material? CBE-30.
- Changing the water system from purified water to WFI? PAS.
- Updating the batch record format? Annual report.
What About Outside the U.S.?
If you sell globally, you’re not just dealing with the FDA. The European Medicines Agency (EMA) uses Type IA, IB, and II changes. Type IA is like the FDA’s annual report - you notify them after the fact. Type IB is like CBE-30, but you can’t ship until they approve it. Type II is PAS. The big difference? EMA doesn’t let you ship after 30 days - you wait for approval. Health Canada is similar to the FDA, but their Level I changes require a 120-day review window. WHO requires a full comparability protocol with stability and bioequivalence data - even for equipment swaps. The ICH Q12 guideline, adopted in 2020, was meant to harmonize these systems. But in practice, companies still have to file separate submissions for each region. There’s no global form. You still need three sets of paperwork.Who Does This Work?
This isn’t a job for one person. It takes a team: quality assurance, manufacturing, validation, regulatory affairs, and sometimes even supply chain. A moderate change can take 120 hours of team time. That’s three weeks of full-time work. Small companies struggle the most. A 2022 FDA survey found only 63% of mid-sized manufacturers had a formal change control system. Large companies like Pfizer use internal risk scoring tools with 15+ criteria. They track every change, every piece of equipment, every supplier. They know exactly what’s PAS, what’s CBE-30, and what’s annual.
What’s Changing in 2026?
The FDA’s 2023 draft guidance on quality risk management is pushing companies to use real-time data - not just batch records - to justify changes. If you’re using sensors to monitor temperature, pressure, or moisture during production, you can use that data to prove your change didn’t affect quality. That could reduce the need for PAS in some cases. Also, continuous manufacturing is becoming more common. If your line runs 24/7 and every step is connected, changing one piece of equipment can ripple through the whole process. That’s almost always PAS. The trend is clear: regulators want proof, not promises. They want data, not paperwork. And they’re watching.What Should You Do Now?
If you’re in pharma manufacturing, here’s what you need to do:- Review every change you made in the last 12 months. Did you classify them correctly?
- Build or update your internal change classification matrix. Use the FDA’s 2021 guidance as a base.
- Train your team. Not just regulators - engineers, operators, and QA staff need to know the difference between CBE-30 and PAS.
- Start collecting real-time process data. It’s not just for efficiency - it’s your future defense.
- If you’re unsure? Call the FDA. Early consultation can save you months - and millions.
Final Thought
Manufacturing changes aren’t about control. They’re about consistency. The medicine your grandmother takes today should be just as safe and effective as the one she took ten years ago. That’s why the rules exist. And that’s why skipping the paperwork isn’t a shortcut - it’s a gamble with patient lives.What happens if I make a manufacturing change without notifying the FDA?
You risk regulatory action. The FDA can issue a warning letter, order a product recall, or even halt distribution of your entire product line. In 2023, 22% of FDA warning letters were tied to unapproved manufacturing changes. Most of these cases involved companies that thought a change was minor but was actually major - like replacing critical equipment without a Prior Approval Supplement.
How do I know if a change is major or minor?
Use risk-based assessment. Ask: Could this change affect the drug’s identity, strength, purity, or potency? If yes, it’s not minor. The FDA’s 2021 guidance includes a table of common changes and their categories. For example, changing the active ingredient’s synthesis pathway is always major. Changing a label font is minor. When in doubt, use a formal tool like FMEA (Failure Modes and Effects Analysis) to score impact and likelihood.
Can I use the same equipment from a different manufacturer?
Only if it’s truly equivalent. The FDA defines equivalent as: same principle of operation, same critical dimensions, same material of construction. Even if the new machine does the same job, if it has a different motor, different cleaning cycle, or different material contact surfaces, it’s a major change requiring a Prior Approval Supplement. Don’t assume - test and document.
Do I need to notify the FDA if I change suppliers for a raw material?
Yes - but the category depends on the material. Changing the supplier of an inactive ingredient like a filler might be a minor change (annual report). Changing the supplier of the active pharmaceutical ingredient (API) is almost always a major change requiring a Prior Approval Supplement. You must show comparability data: stability, purity, dissolution, and potency across batches from both suppliers.
How long does it take to get FDA approval for a major change?
A Prior Approval Supplement (PAS) typically takes 6 to 12 months for review. The FDA may request additional data or clarification, which can extend the timeline. If you’re working on a critical product, you can request a priority review, but this is rare and requires strong justification. Plan ahead - don’t wait until you’re ready to make the change to start the paperwork.
Is there a global standard for manufacturing change notifications?
There’s no single global standard, but the ICH Q12 guideline (2020) aims to harmonize requirements across the U.S., EU, Canada, Japan, and others. In practice, each region still has its own rules. The FDA uses PAS/CBE-30/annual, the EMA uses Type IA/IB/II, and Health Canada uses Level I/II/III. Companies selling worldwide must file separate submissions for each region, even if the change is identical.
What documents do I need to support a manufacturing change?
You need validation reports, comparative batch data (at least three batches), facility diagrams, equipment specifications, cleaning validation records, and stability study results. For major changes, you must show that the new process produces a product equivalent in quality to the original. The FDA’s Manufacturing Site Change Supplements guidance (FDA-2015-N-3454) outlines these requirements in detail.
Can I implement a change immediately if it’s a CBE-30?
Yes - but only after you’ve submitted the CBE-30 notification and waited 30 days. You cannot ship the changed product until the 30-day period has passed, even if the FDA hasn’t responded. The 30-day window is your legal buffer. If the FDA disagrees with your classification, they can require you to stop distribution - but you’re not breaking the law by proceeding after 30 days.





One comment
Man, I’ve seen so many teams cut corners on these changes thinking it’s ‘just a pump swap’ - then boom, FDA comes knocking with a recall notice. It’s not that hard to fill out a form. If your QA team can’t handle 30 minutes of paperwork, maybe they shouldn’t be touching equipment at all. 😅
bro just use FMEA bro. if score >100 = PAS. no brain needed. i did this for 3 diff plants in india. saves so much stress. also train ur operators. they notice stuff before QA lol
Let’s be honest - this whole system is a bureaucratic farce designed to keep mid-tier manufacturers from innovating. The FDA doesn’t care about patient safety; they care about liability coverage. A change in cleaning protocol for a non-critical component? That’s not a risk - it’s a compliance tax. And don’t get me started on the 120-hour ‘team effort’ for a CBE-30. If you’re not a Fortune 500 company with a regulatory department the size of a small country, you’re just playing whack-a-mole with paperwork. Real innovation happens in the shadows, where people actually make medicine, not file forms.