Postpartum depression isn’t just feeling sad after having a baby
It’s a real medical condition that affects about 1 in 8 new mothers. Unlike the baby blues, which fade in a week or two, postpartum depression sticks around. It makes it hard to sleep, eat, bond with your baby, or even get out of bed. And if you’re breastfeeding, the question isn’t just “Should I take medicine?” - it’s “Which medicine won’t hurt my baby?”
Medication isn’t the enemy - untreated depression is
Many moms worry that taking antidepressants while breastfeeding means they’re poisoning their child. But the truth is, the biggest risk isn’t the medicine - it’s the depression itself. Untreated postpartum depression can lead to poor feeding, delayed development in babies, and even long-term emotional struggles for both mother and child. Major medical groups like the American College of Obstetricians and Gynecologists (ACOG) and the CDC agree: the benefits of treating depression almost always outweigh the tiny risks of medication passing into breast milk.
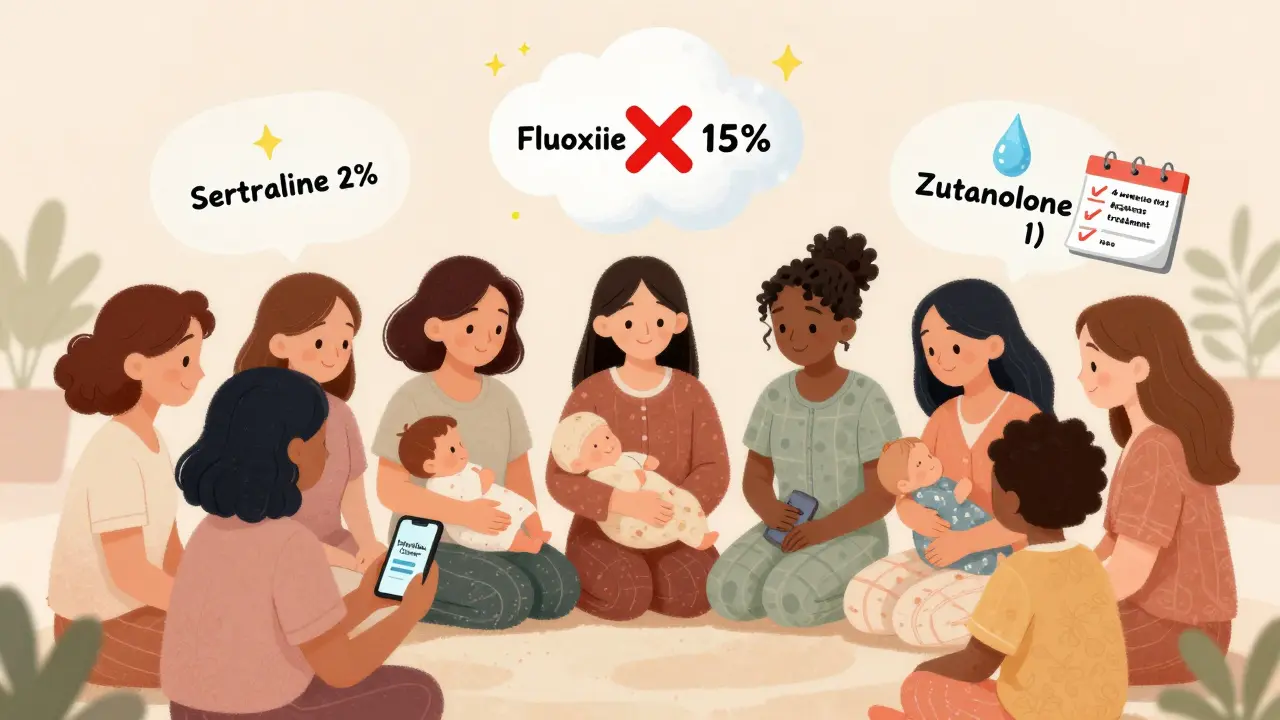
Not all antidepressants are the same when you’re nursing
Some drugs slip into breast milk easily. Others barely make it through. The key is understanding how much actually reaches your baby - measured as a percentage of your dose, adjusted for their weight. This is called the Relative Infant Dose (RID). Anything under 10% is generally considered safe.
- Sertraline (Zoloft): Only 0.5-3.2% of your dose gets into breast milk. In over 1,800 mother-baby pairs studied, 92% of infants had undetectable levels. Most moms report no issues. It’s the #1 recommended choice.
- Paroxetine (Paxil): Slightly higher transfer (0.9-8.6%), but still low. Fewer side effects in babies than other SSRIs. Good option if sertraline doesn’t work.
- Citalopram (Celexa): Transfer rate is 3.5-8.9%. Watch for higher doses - over 40mg daily might affect heart rhythm in rare cases.
- Fluoxetine (Prozac): Avoid if you can. It transfers at 5.9-15.2% and sticks around in your baby’s system for weeks because of its long half-life. One mom reported her daughter had explosive diarrhea until she switched off fluoxetine.
- Venlafaxine (Effexor): Transfer is low (1.4-5.9%), but higher doses (above 150mg) have been linked to fussiness and sleep problems in babies.
- Bupropion (Wellbutrin): Can increase seizure risk in infants. Not recommended unless other options fail.
- Doxepin: Avoid completely. There are documented cases of infants developing apnea and turning blue at low maternal doses.
What side effects should you watch for in your baby?
Most babies show no signs at all. But in the first 2-4 weeks after you start a new antidepressant, keep an eye out for:
- Excessive sleepiness or trouble waking for feeds
- Poor feeding or refusing the breast
- Unusual fussiness or crying that doesn’t stop
- Changes in bowel movements - diarrhea or constipation
- Restlessness or jitteriness
If you notice any of these, don’t panic. Call your doctor. Often, lowering the dose or switching medications helps. One mom on a breastfeeding forum shared: “My baby got super gassy and fussy on sertraline. We dropped from 100mg to 50mg, and within 3 days, he was back to his sweet self.”
Timing matters more than you think
There’s a simple trick to reduce your baby’s exposure even further: take your pill right after breastfeeding. That way, the drug concentration in your milk is lowest when your baby feeds again. For most medications, peak levels happen 1-3 hours after taking the pill. Waiting 3-4 hours before the next feed cuts exposure significantly.
Some moms also pump and dump after taking a dose - but that’s rarely necessary. For sertraline and paroxetine, it’s overkill. For fluoxetine? Maybe. But even then, the benefit is minimal. Talk to your provider before doing this - it can hurt your milk supply and add unnecessary stress.
New treatments like zuranolone: promising, but still unclear
In August 2023, the FDA approved zuranolone (Zurzuvae), the first pill made specifically for postpartum depression. It works fast - half the women in trials felt better in under two weeks. But here’s the catch: the original study required moms to stop breastfeeding. The label still says, “There are no data on human milk.”
However, early data from LactMed suggests zuranolone passes into breast milk at very low levels - only 0.5-1.5% of the maternal dose. Some experts believe it’s likely safe, but the official recommendation is still to pump and discard milk for one week after the last dose. If you’re considering this drug, ask your doctor about the latest research. It’s new, and guidelines are still catching up.
What about therapy, exercise, or supplements?
Medication isn’t the only path. Many moms find relief with:
- Therapy: Cognitive behavioral therapy (CBT) and interpersonal therapy (IPT) are proven to help PPD. Some insurance plans cover it for new moms.
- Support groups: Postpartum Support International has free online groups. Talking to other moms who get it can be life-changing.
- Exercise: Even 20 minutes of walking a day can boost mood. You don’t need a gym - just get outside with your baby in the stroller.
- Omega-3s and vitamin D: Low levels are linked to higher depression risk. Talk to your doctor about testing and supplementing if needed.
But here’s the thing: therapy and lifestyle changes take time. If you’re struggling to get out of bed, eat, or hold your baby without crying - you need help now. Medication can give you the stability to start doing the other things that heal you.

How do you know if it’s working?
Antidepressants don’t kick in overnight. Most moms start noticing small changes after 2-3 weeks. Real improvement usually takes 4-6 weeks. Don’t quit because you don’t feel better right away. Stopping suddenly can make depression worse - and increase your chance of relapse by three times.
Use the Edinburgh Postnatal Depression Scale (EPDS). It’s a simple 10-question test your OB or pediatrician should give you at your 1-, 2-, 4-, and 6-month checkups. If your score is 13 or higher, you likely have PPD. Track your score over time. It’s the best way to know if your treatment is working.
What if you’re still scared?
You’re not alone. A 2021 survey of 347 breastfeeding moms with PPD found that 78% took antidepressants. Of those, 86% said their babies showed no noticeable side effects. But 12% stopped because they thought something was wrong. In most cases, the issue wasn’t the medicine - it was anxiety.
That’s why it’s so important to have a trusted provider. The InfantRisk Center runs a hotline (806-352-2519) staffed by pharmacists who specialize in breastfeeding and meds. They answer 3,000 calls a month. You don’t have to guess. Call them. Bring your prescription. Ask: “Is this safe for my baby?”
Bottom line: You deserve to feel like yourself again
There’s no shame in needing help. You didn’t fail because you have postpartum depression. You’re not a bad mom because you’re taking medicine. In fact, taking care of your mental health is one of the most loving things you can do for your baby.
Sertraline is the safest, most studied option. Paroxetine is a close second. Avoid fluoxetine and doxepin. Watch your baby for the first few weeks. Talk to your doctor. Use support tools. And remember - healing isn’t about being perfect. It’s about showing up, even on the hard days. Your baby needs you, not a perfect version of you. A real, tired, sometimes anxious, but treated and healing you? That’s the mom your baby needs.
Can I breastfeed while taking sertraline?
Yes. Sertraline is the most recommended antidepressant for breastfeeding moms. Less than 3.2% of your dose enters breast milk, and in most cases, babies show no side effects. Over 1,800 mother-baby pairs in studies showed no harm. It’s considered safe and effective.
Will antidepressants make my baby sleepy or fussy?
Some babies might be slightly sleepier or fussier in the first 2-4 weeks after you start a new medication, especially with higher doses. But these effects are rare with sertraline and paroxetine. If they happen, they usually go away on their own. If they don’t, talk to your doctor - a small dose change often fixes it.
Is it safe to take fluoxetine while breastfeeding?
Fluoxetine is not recommended. It transfers into breast milk at higher levels (up to 15%) and builds up in your baby’s system because it stays in the body for weeks. There are documented cases of infants developing irritability, poor feeding, and even diarrhea. If you’re currently on fluoxetine and breastfeeding, talk to your doctor about switching to sertraline.
How long does it take for antidepressants to work while breastfeeding?
Most moms start noticing small improvements in mood after 2-3 weeks. Full benefits usually take 4-6 weeks. Don’t stop because you don’t feel better right away. Stopping too soon increases your risk of relapse by three times. Give it time, and track your progress with the EPDS questionnaire.
Can I take zuranolone (Zurzuvae) while breastfeeding?
The FDA hasn’t approved zuranolone for use while breastfeeding because the original trials required moms to stop nursing. However, early data shows it passes into milk at very low levels (0.5-1.5%). Some experts believe it’s likely safe, but the official recommendation is to pump and discard milk for one week after the last dose. Talk to your doctor about whether this new treatment is right for you.
What if my baby has side effects? Should I stop the medicine?
Don’t stop without talking to your doctor. Many side effects are mild and temporary. Often, lowering the dose or switching to a different medication (like from fluoxetine to sertraline) solves the problem. Stopping abruptly can make your depression worse and put you at higher risk of relapse. Your doctor can help you find a safer option.
Where can I get reliable information about medications and breastfeeding?
The best free resource is LactMed, run by the National Library of Medicine. It’s updated weekly and gives detailed data on over 1,300 drugs. You can also call the InfantRisk Center at 806-352-2519. They’re pharmacists who specialize in breastfeeding and meds - they answer over 3,000 calls a month.




One comment
I appreciate the data on RID percentages. Most moms don’t realize how little actually gets into milk. Sertraline’s 0.5-3.2% is practically negligible. I wish more OBs would cite LactMed instead of just saying 'it’s fine.'
This is exactly what I needed. I was terrified to start meds but kept crying while feeding my daughter. Sertraline changed everything. She’s 6 months now and still smiles when I pick her up. 🥹
Let’s be real-this is Big Pharma whispering in your ear while your baby sleeps. Fluoxetine’s long half-life? That’s not a side effect, that’s a chemical hostage situation. They want you addicted.
The RID metric is underutilized in clinical practice. Most providers default to fluoxetine because it’s cheap and insurance-friendly. Meanwhile, sertraline’s pharmacokinetic profile is objectively superior for lactation. The fact that this isn’t standard of care is a systemic failure.
Ah yes, the sacred text of maternal pharmacology-written by a committee that’s never held a screaming newborn at 3 a.m. while their own cortisol levels are in orbit. Sertraline? Cute. But have you considered the epigenetic ripple effects? The baby’s microbiome? The unspoken trauma of chemical intervention? We’ve pathologized grief and sold it as a pill.
I must express my profound concern regarding the normalization of pharmaceutical intervention during the sacred lactation window. The subtle, insidious erosion of natural maternal bonding through synthetic neurochemical modulation is not merely a medical concern-it is a civilizational decline.
Sertraline = good. Fluoxetine = bad. Pump and dump = overkill. 🤍
To anyone reading this and feeling guilty: you’re not failing. You’re fighting. And if taking a pill helps you hold your baby without shaking? That’s not weakness. That’s courage. You’re already doing better than you think.
Let’s not ignore the elephant in the room: the FDA’s approval of zuranolone was rushed. The study that excluded breastfeeding mothers? That’s not science-it’s liability management. They’re selling a miracle drug while burying the data. The 0.5-1.5% transfer rate? That’s a guess. A very expensive guess.
I’m a dad. My wife was on sertraline. Our son had zero side effects. What I saw was a woman coming back to life. The real tragedy isn’t the medication-it’s the stigma that makes mothers feel like monsters for needing help.
Bro, sertraline is the GOAT for nursing moms. I’m from India, my sister took it, baby was chill. Even her mom said ‘beta, yeh dawa toh sahi hai’ 😅. Avoid fluoxetine like the plague. Also, walk outside daily. Sunlight + baby = free therapy.
I took Zoloft while breastfeeding my twins. One had mild gas, the other slept like a rock. We dropped the dose from 100 to 50 and boom-both were happy. Stop overthinking. Your baby doesn’t care if you’re on meds. They care if you’re present.
The notion that antidepressants are ‘poison’ is a relic of patriarchal pseudoscience. We have over two decades of longitudinal data demonstrating that maternal mental health stabilization yields superior neurodevelopmental outcomes in infants. To frame medication as a moral compromise is to weaponize guilt against the vulnerable. This isn’t pharmacology-it’s oppression dressed in lactation advice.
I just wanted to say thank you for this post. My wife started sertraline last month and i’ve seen her smile again. I know it’s not perfect, but it’s real. We’re learning. And that’s enough. (sorry for typos-tired dad here 😴)