Kidney Hydration Calculator
Personal Hydration Assessment
This tool calculates your appropriate hydration protocol for contrast dye procedures based on your kidney function and risk factors.
Recommended Hydration Plan
When you're getting a CT scan, angiogram, or other imaging test that uses contrast dye, most people don't think about their kidneys. But if you have even mild kidney trouble, that dye can cause real damage. This isn't rare. About 1 in 10 people who get contrast dye end up with some level of kidney injury-especially if they're over 60, have diabetes, or already have reduced kidney function. The good news? You don't have to accept this risk. A simple, well-timed hydration plan can cut your chances of kidney damage by more than half. And it’s not just about drinking more water.
Why Hydration Matters for Kidneys on Medications
Contrast dye used in imaging tests is a known nephrotoxin. It doesn’t poison your kidneys like poison does-it stresses them. The dye thickens the fluid inside the kidney’s filtering tubes, reduces blood flow to those areas, and creates oxidative stress. The result? Acute kidney injury, called contrast-induced acute kidney injury (CI-AKI). It’s not always obvious. You might not feel sick. But your creatinine levels will rise, and your kidneys will work harder to recover-if they can.
Studies show CI-AKI increases hospital stays by over three days and adds nearly $7,500 to your bill. For someone with chronic kidney disease, it can mean the difference between managing their condition and needing dialysis. That’s why hydration isn’t optional. It’s a shield. The goal? Keep blood flowing through your kidneys, flush out the dye faster, and reduce how long it lingers in sensitive tissues.
The Science Behind Hydration Protocols
Not all hydration is created equal. A 2020 analysis of 60 clinical trials involving over 21,000 patients found that the type, timing, and amount of fluid matter more than you’d think.
The most common method is intravenous (IV) saline-0.9% sodium chloride. The standard protocol? Start 4 hours before the procedure and continue for 4 hours after, at a rate of 3 to 4 mL per kilogram of body weight per hour. For a 70 kg person, that’s about 210 to 280 mL per hour. That’s more than a full water bottle every hour.
But there’s a better way. A more advanced method uses sodium bicarbonate instead of saline. It’s not just about volume-it’s about pH. Bicarbonate helps neutralize the acidic environment created by the dye, reducing oxidative damage. Studies show it cuts CI-AKI risk by 26% compared to no hydration. Not bad, but it’s not the top performer.
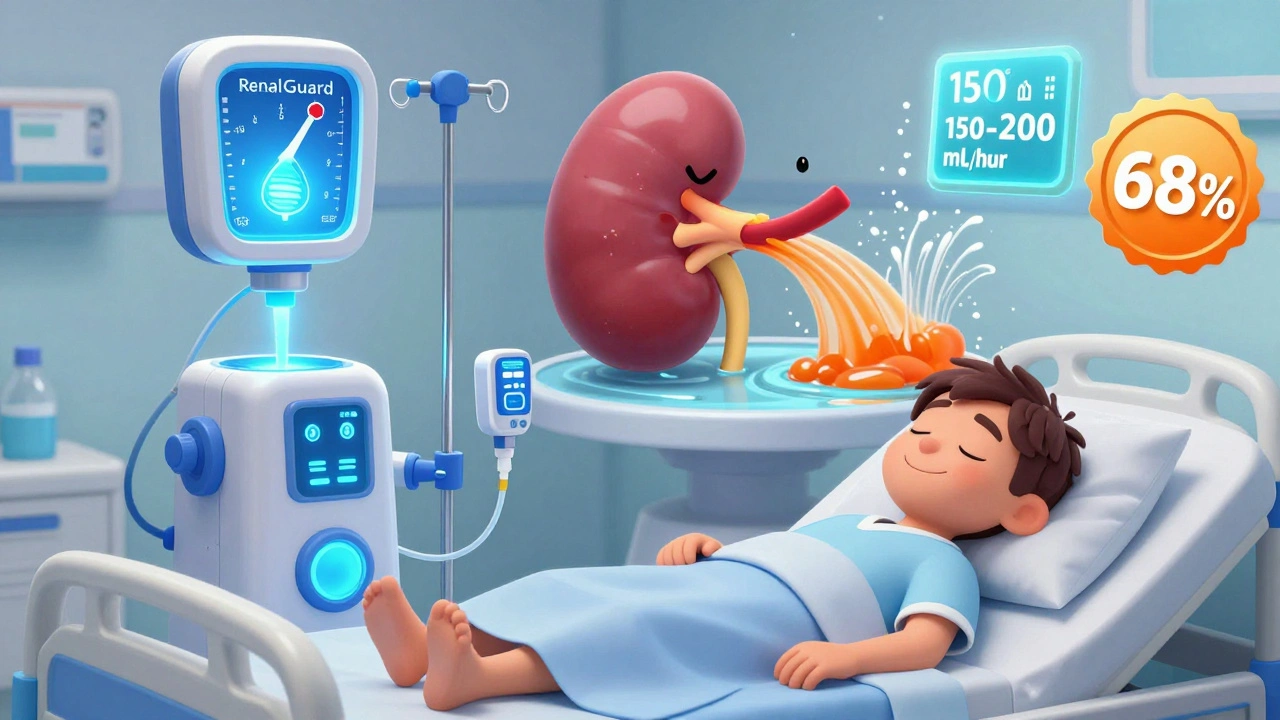
The most effective? The RenalGuard system. This isn’t just an IV drip. It’s a closed-loop machine that monitors your urine output in real time and adjusts fluid delivery to keep you peeing at 150-200 mL per hour. That’s the sweet spot. Too little, and dye stays too long. Too much, and you risk fluid overload-especially dangerous if you have heart failure. RenalGuard reduced CI-AKI by 68% in high-risk patients. That’s not a small win. That’s life-changing.
Who Needs Aggressive Hydration-and Who Doesn’t
Not everyone needs IV fluids. If your kidney function is normal (eGFR above 60 mL/min/1.73m²), drinking water is likely enough. A 2018 study showed that patients with eGFR above 29 mL/min/1.73m² had no difference in kidney injury rates whether they got IV fluids or just drank water.
Here’s the breakdown:
- eGFR above 60: Oral hydration (500 mL water 2 hours before, 250 mL per hour during) works just as well as IV. No need for needles.
- eGFR 30-59: You’re in the danger zone. IV isotonic saline at 1-1.5 mL/kg/hour for 3-12 hours before and after is recommended by the 2025 VA/DOD guidelines.
- eGFR below 30: Contrast dye should be avoided if possible. If absolutely necessary, use RenalGuard or hemodynamic-guided hydration under close supervision.
And don’t forget heart failure. Aggressive hydration can backfire here. Too much fluid can cause pulmonary edema. If you’ve been told to limit fluids because of your heart, your care team needs to balance kidney protection with heart safety. A 500 mL excess might be the difference between a smooth recovery and a trip to the ER.
Oral vs. IV Hydration: What Works Best
Many patients worry about IV lines. They’re uncomfortable. They limit mobility. They cost more. But does drinking water really help?
Yes. Multiple studies show oral hydration is noninferior to IV for low- to moderate-risk patients. One trial compared 4.7% CI-AKI in the oral group to 5.1% in the IV group-no statistically significant difference. For someone with eGFR above 40, sitting with a water bottle for a few hours is just as effective as being hooked up to an IV pole.
But here’s the catch: compliance. People forget. They get nervous before a procedure. They don’t drink enough. That’s why IV is still preferred in hospitals-it’s controlled. At home, you’re on your own. If you’re doing oral hydration, set alarms. Drink 250 mL every hour. No skipping. Use a marked bottle. Track it.
Advanced Systems: RenalGuard and Beyond
RenalGuard isn’t science fiction. It’s FDA-approved and used in over 15% of high-volume cardiac labs in the U.S. It’s a machine that connects to your IV line and a urine collection bag. Sensors measure output every few minutes. If you’re not peeing enough, it automatically increases fluid. If you’re peeing too much, it slows down. It’s like cruise control for your kidneys.
For patients with eGFR under 60, the numbers speak for themselves: CI-AKI dropped from 22.1% without it to just 7.3% with RenalGuard. That’s a 65% reduction. The catch? It costs about $1,200 more per procedure. But when you factor in the $7,500 average cost of treating CI-AKI, it pays for itself-and then some.
Other advanced systems use central venous pressure monitoring to adjust fluids based on heart pressure. These are mostly used in research settings now, but they’re the future. The American Heart Association predicts AI-driven fluid systems will be standard within five years. These systems will analyze your age, kidney function, heart status, and even your weight changes during the procedure to fine-tune hydration in real time.
What Your Care Team Should Do
Before your imaging test, ask:
- What’s my eGFR? (It should be checked within 30 days of the procedure.)
- Do I need IV fluids, or is water enough?
- Will you monitor my urine output during the procedure?
- Do you use RenalGuard or similar systems for high-risk patients?
Don’t assume your doctor knows your kidney numbers. If you’re on blood pressure meds, diuretics, or metformin, tell them. Those can affect how your kidneys handle contrast. If you’ve had kidney injury before, say so. This isn’t just about one scan-it’s about protecting your long-term kidney health.
Hospitals that standardized hydration protocols cut CI-AKI rates in half. The Mayo Clinic dropped theirs from 12.3% to 5.7% in a year by making hydration mandatory and tracking outcomes. It’s not magic. It’s policy. You have the right to ask if your facility has one.

What You Can Do Today
Even if you’re not scheduled for a scan yet, you can prepare:
- Know your eGFR. Request it from your doctor if it’s not in your records.
- Keep a water bottle with you. Aim for 1.5-2 liters a day unless told otherwise.
- Avoid NSAIDs (like ibuprofen) 24-48 hours before a scan. They reduce kidney blood flow.
- If you’re diabetic, don’t take metformin the day of the scan unless cleared by your doctor. It can build up if your kidneys are stressed.
And if you’re told you need IV hydration? Don’t push back just because it’s inconvenient. That hour or two of sitting with an IV could save you months of dialysis, extra doctor visits, and hospitalizations.
What Doesn’t Work
There’s a lot of noise out there. N-acetylcysteine (NAC) was once thought to protect kidneys. But the 2020 meta-analysis showed no benefit when used with proper hydration. Same with caffeine, antioxidants, or herbal supplements. None of them replace fluid volume. Don’t waste your time or money.
And don’t rely on “just drink water” as a catch-all. If you’re high-risk, that’s not enough. You need the right fluid, at the right time, at the right rate.
Final Thoughts
Protecting your kidneys from nephrotoxic medications isn’t about being scared. It’s about being informed. You have more control than you think. Whether it’s choosing to drink water instead of getting an IV, asking for RenalGuard, or simply knowing your eGFR-you’re not powerless.
The best hydration plan isn’t the most expensive one. It’s the one that fits your body, your risk, and your life. Ask the questions. Demand the data. And don’t let a routine scan become a turning point you didn’t see coming.
Can drinking water really protect my kidneys from contrast dye?
Yes, for people with mild to moderate kidney function (eGFR above 30 mL/min/1.73m²), drinking water before and after a scan works just as well as IV fluids. Studies show no significant difference in kidney injury rates between those who drank 500 mL two hours before and 250 mL per hour during the procedure, and those who got IV saline. But if your kidney function is low, IV hydration is safer and more reliable.
Is IV hydration always necessary before a CT scan?
No. If your eGFR is above 60 and you have no other risk factors like diabetes or heart failure, oral hydration is sufficient. For eGFR between 30 and 59, guidelines recommend IV isotonic saline. For eGFR below 30, contrast dye should be avoided unless absolutely necessary, and if used, advanced hydration like RenalGuard is preferred.
What is the RenalGuard system, and is it worth it?
RenalGuard is a closed-loop system that automatically adjusts IV fluid based on your real-time urine output. It targets 150-200 mL/hour to flush out contrast dye efficiently. In high-risk patients, it reduces kidney injury by 68% compared to no hydration. While it costs about $1,200 more per procedure, it saves an average of $4,200 by preventing hospital stays and dialysis. It’s worth it for patients with chronic kidney disease or heart failure.
Can I take my regular meds before a scan with contrast dye?
It depends. Avoid NSAIDs like ibuprofen for 24-48 hours before the scan-they reduce kidney blood flow. If you take metformin for diabetes, you’ll usually need to skip it the day of the scan and wait 48 hours after to restart, to avoid lactic acidosis if your kidneys are stressed. Diuretics may be held temporarily. Always check with your doctor before stopping any medication.
Does hydration help with other nephrotoxic medications besides contrast dye?
Yes. Hydration is also recommended for drugs like vancomycin, aminoglycosides, and certain chemotherapy agents that can harm the kidneys. The principle is the same: keep blood flowing through the kidneys and dilute the drug to reduce its toxic concentration. Always ask your pharmacist or doctor if your meds require extra fluids.





One comment
My cousin got contrast dye last year and ended up in the hospital with kidney issues. No one told him anything about hydration. He just drank a bottle of water and thought that was enough. Turned out his eGFR was 38. Should’ve been on IV. Hospitals are lazy about this stuff.
Of course they don’t tell you this. Big Pharma doesn’t want you drinking water instead of paying for expensive IVs and machines. RenalGuard? That’s just another way to make you pay more while they profit. They’d rather you stay sick than save you with a damn water bottle.
It is fascinating how the medical-industrial complex has weaponized hydration protocols as a revenue stream. The RenalGuard system, while statistically impressive, represents a paradigm of technological overreach-a solution in search of a problem that could be solved with basic physiology and patient education. One must ask: Is this innovation or institutionalized commodification of bodily function?
Good stuff. I work in radiology and we’ve switched to mandatory eGFR checks before contrast. If you’re above 60, we hand you a liter of water and a timer. If you’re below, we use IV. Simple. No drama. And yeah, we use RenalGuard for heart failure patients now. Worth every penny. 🙌
Why are we letting the government dictate how much water we drink? This is socialist medicine. If I want to skip the IV and just chug Gatorade, that’s my right. They’re just trying to control us with these protocols. Also, who made the FDA the boss of my kidneys?
I just had a CT last week and asked for the hydration plan. They gave me a water bottle and said ‘drink this before and after.’ Did it. Felt fine. No IV. No problems. Simple works.
Wait-so you’re telling me that a machine that measures how much I pee… is better than just drinking water? That’s not science-that’s surveillance. They’re tracking my urine output now? Next they’ll be microchipping us to monitor hydration levels. This is dystopia disguised as medicine.
For patients with CKD, this is non-negotiable. The RenalGuard system isn’t just a device-it’s a paradigm shift in nephroprotection. Real-time, closed-loop fluid management reduces variability, eliminates human error, and aligns with precision medicine principles. The cost-benefit analysis is unequivocal: $1,200 upfront prevents $7,500 in downstream costs and potential ESRD. This isn’t luxury-it’s clinical necessity.
My mom got contrast dye last year and they didn’t even check her eGFR. She’s 72, diabetic, and now she’s on dialysis 3x a week. I’m so mad. Why didn’t anyone tell us? 😔 I wish I’d known about this sooner. This post should be mandatory reading.
I’ve been telling my patients this for years. Water is powerful. You don’t need a machine if you’re not high risk. Just drink. Slowly. Regularly. It’s not complicated. And if you’re scared, ask your doctor. No one should feel alone with this.
STOP WAITING FOR A SCAN TO CARE ABOUT YOUR KIDNEYS! Start drinking water daily. Stop taking ibuprofen like candy. Know your eGFR. This isn’t just about contrast-it’s about your whole life. You can fix this now. Don’t wait until it’s too late. You got this 💪
They call it ‘contrast-induced injury’ like it’s some mysterious curse. Nah. It’s just the hospital being lazy and charging you $2,000 for a saline drip you could’ve gotten for free at home. The real nephrotoxin? The healthcare system.
Let’s be honest: the RenalGuard system is a glorified IV pump with a urine sensor. The 68% reduction? Likely inflated by selection bias-only the sickest patients get it, and those are the ones who would’ve had the worst outcomes anyway. The data looks good because they cherry-picked the high-risk cohort. Classic.
I didn’t know my eGFR until last month. My doctor never told me. I’m 65 and have high blood pressure. I’m going to ask for it before my next scan. Thank you for this. I feel more in control now.
It is regrettable that the public discourse surrounding nephroprotection has been reduced to a binary of IV versus oral hydration. The underlying issue-the erosion of clinical judgment in favor of protocolized medicine-remains unaddressed. One must question whether the emphasis on quantifiable metrics has supplanted the art of patient-specific care.