Coronary artery disease (CAD) isn’t just a buzzword in medical journals-it’s the number one killer worldwide. According to the World Health Organization, ischemic heart disease, mostly caused by CAD, accounted for 13% of all deaths between 2000 and 2021. That’s more than 1 in 8 deaths globally. And it’s not just happening to older people. More and more adults in their 40s and 50s are being diagnosed, often after a heart attack has already happened. The truth? Most cases develop slowly, silently, over decades. By the time symptoms show up, the damage is often advanced. But here’s the good news: you can stop it. You can slow it. You can even reverse some of it-if you know what to look for and what to do.
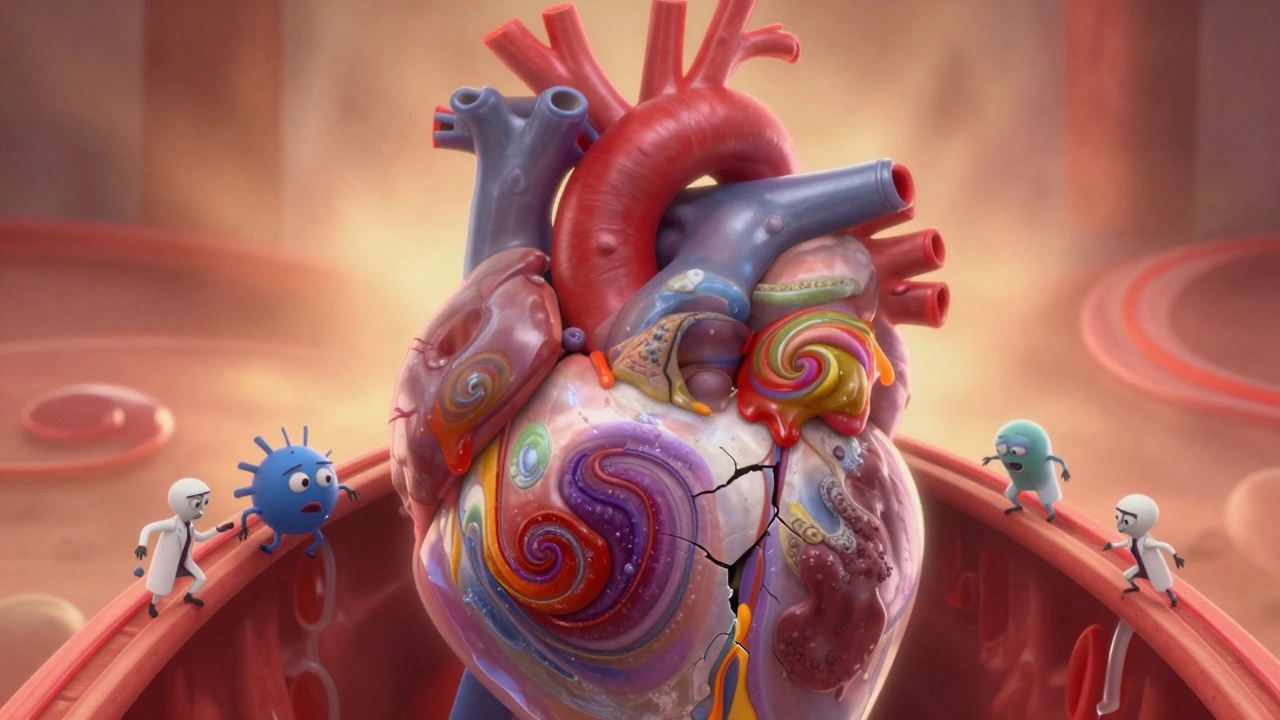
What Exactly Is Atherosclerosis?
Atherosclerosis is the root cause of coronary artery disease. It’s not just "clogged arteries" like a pipe full of rust. It’s a complex, living process inside your blood vessels. Fatty deposits-mainly cholesterol, especially LDL-start sticking to the inner walls of your coronary arteries. These aren’t just blobs of fat. They trigger inflammation. Immune cells rush in, try to clean it up, and get trapped. Over time, this builds up into something called a plaque. Plaques can be soft and dangerous, or hard and stable.
Unstable plaques are the real killers. They have a thin outer shell, a big oily core, and lots of inflammatory cells. They don’t always block more than half the artery. Sometimes they’re only 30% narrowed. But because they’re so fragile, they can rupture suddenly. When that happens, your body tries to patch it with a blood clot-and that clot can completely block the artery. That’s when a heart attack happens.
Stable plaques are different. They’re thicker, harder, calcified. They may block 70% or more of the artery, but they don’t rupture easily. People with these often feel chest pain during exercise-stable angina-because the heart isn’t getting enough oxygen under stress. But at rest, they’re fine. These plaques are dangerous too, but they’re predictable. That’s why doctors can plan treatment around them.
Who’s at Risk? The Real Culprits Behind CAD
You can’t change your age or your genes. But you can change most of what actually leads to heart disease. The 2023 ACC/AHA guidelines break down risk factors into clear categories. High blood pressure? Check. High cholesterol? Check. Smoking? Big check. Diabetes? Major red flag.
Here’s what actually matters:
- Smoking: Even one cigarette a day raises your risk. The chemicals damage the lining of your arteries and make plaques more likely to rupture.
- High LDL cholesterol: LDL is the "bad" cholesterol that builds plaques. Levels above 160 mg/dL are dangerous. But even levels between 100 and 130 can be risky if you have other problems.
- Diabetes: People with type 2 diabetes have the same heart attack risk as someone who’s already had one. High blood sugar damages blood vessels over time.
- Obesity: Especially belly fat. A BMI over 30 increases your risk by 40%. Fat tissue releases inflammatory chemicals that speed up plaque growth.
- Physical inactivity: Sitting for more than 8 hours a day raises your risk as much as smoking. Movement keeps your arteries flexible and your blood pressure down.
- Family history: If a parent had heart disease before age 55, your risk doubles. But that doesn’t mean it’s inevitable-it just means you need to be extra careful.
Here’s something most people don’t know: high-risk patients often have more than one of these. In fact, 60% of people with CAD have at least three major risk factors. And 75% of heart attacks happen in this group. That’s why doctors now classify risk into three levels: low (<1% chance of heart attack per year), intermediate (1-3%), and high (>3%). If you’re in the high-risk group, you need aggressive treatment-not just a statin and a pat on the back.

How Is CAD Diagnosed? Beyond the Stereotype
Most people think a heart attack is the first sign of CAD. But that’s not true. By the time someone has a heart attack, the disease has been growing for 10, 20, even 30 years. The goal now is to catch it before it’s too late.
Here’s how it’s done:
- Electrocardiogram (ECG): This simple test records your heart’s electrical activity. It can show if you’ve had a past heart attack or if your heart is under strain. It’s quick, painless, and done in most GP offices.
- Stress tests: You walk on a treadmill or ride a stationary bike while your heart is monitored. If your arteries are narrowed, your heart won’t get enough oxygen during exercise-and that shows up on the ECG or imaging. Newer versions use ultrasound or nuclear scans for better accuracy.
- Coronary angiography: This is the gold standard. A thin tube is threaded from your wrist or groin into your heart. Dye is injected, and X-rays show exactly where blockages are. It’s invasive, but it’s the only way to see the exact size and location of plaques.
- Ankle-Brachial Index (ABI): This test compares blood pressure in your ankle to your arm. If it’s low, you likely have plaque in your leg arteries too-which means you probably have it in your heart. About 40% of people with CAD also have peripheral artery disease. This test is cheap, quick, and often skipped-but it shouldn’t be.
Doctors are also starting to use CT scans to look for calcium in your coronary arteries. A high calcium score means you have a lot of plaque-even if you feel fine. It’s not for everyone, but if you’re in the intermediate risk group, it can help decide whether you need stronger meds.
Treatment: It’s Not Just Pills and Surgery
Treatment for CAD isn’t one-size-fits-all. It’s layered. Lifestyle changes come first. Always. Then meds. Then procedures-only if needed.
Lifestyle changes are the most powerful tool you have. The 2023 guidelines say this clearly: no amount of medication can fully replace healthy habits. A heart-healthy diet means more vegetables, whole grains, fish, nuts, and less sugar, processed meat, and fried food. The Mediterranean diet has been proven to reduce heart attacks by 30%. Exercise? At least 150 minutes a week of brisk walking. That’s 30 minutes, five days a week. You don’t need to run a marathon. Just move more than you sit.
Medications are the next step:
- Statins: These lower LDL cholesterol by 30-50%. They also stabilize plaques, making them less likely to rupture. Most people with CAD need to take them for life.
- Aspirin: Used to prevent clots. Not for everyone-only if your risk is high enough. It can cause bleeding, so don’t start it without your doctor’s advice.
- Beta-blockers: Slow your heart rate and lower blood pressure. They reduce chest pain and lower the chance of another heart attack.
- ACE inhibitors or ARBs: Help your heart relax and lower blood pressure. Especially important if you have diabetes or heart failure.
- PCSK9 inhibitors: Newer injectable drugs for people who can’t get their LDL low enough with statins alone. They can drop LDL by 60%.
Procedures are for when meds and lifestyle aren’t enough:
- Percutaneous Coronary Intervention (PCI): Also called angioplasty. A balloon is inflated in the blocked artery, and a metal mesh stent is left behind to keep it open. It’s done through a tiny puncture in the wrist. Most people go home the next day.
- Coronary Artery Bypass Grafting (CABG): Open-heart surgery. A vein or artery from another part of your body is used to go around the blockage. It’s more invasive, but for people with multiple blockages or diabetes, it lasts longer than stents.
There’s no magic fix. But if you combine all three-lifestyle, meds, and procedures when needed-you can live a full, active life with CAD.

The Future: Personalized Care and Cardio-Oncology
The biggest shift in CAD care isn’t a new drug-it’s a new mindset. Doctors are moving away from treating "heart disease" as one thing. Now they’re looking at you as a whole person.
For example, if you have cancer and CAD, you’re in a new category called cardio-oncology. Chemo can damage your heart. Radiation can scar your arteries. So now, oncologists and cardiologists work together before treatment even starts. They check your heart health, adjust meds, and plan around risks.
Another big change: risk assessment is more precise. Instead of guessing if you’re "high risk," doctors now use tools that combine your cholesterol, blood pressure, age, smoking status, diabetes, and even family history into a single score. That score tells them exactly how aggressive your treatment should be.
And research is moving toward plaque stabilization-not just opening arteries. New drugs are being tested to reduce inflammation inside plaques. Some are already in use, like colchicine, a cheap anti-inflammatory that’s shown to cut heart attacks by 30% in high-risk patients.
The message is clear: CAD isn’t a death sentence. It’s a chronic condition-like diabetes or high blood pressure. And like those, it can be managed well if you act early, stay consistent, and work with your doctor.
What Happens If You Ignore It?
Ignoring CAD doesn’t mean nothing happens. It means things happen slowly-until they don’t.
Left untreated, plaques grow. Arteries narrow. Chest pain becomes more frequent. Then comes a heart attack. After that, your heart muscle weakens. You might develop heart failure-where your heart can’t pump well enough to meet your body’s needs. You could need a transplant. Or you could die suddenly, without warning.
And the costs? The American Heart Association says cardiovascular diseases will cost $1.1 trillion a year by 2035. Most of that is CAD. But the human cost is even higher. Families lose parents. Kids lose mothers. Workers lose their ability to do what they love.
You don’t have to be part of that number.



One comment
Just read this after my dad’s stent procedure-thank you for laying it out so clearly. I finally get why he’s so serious about walking every morning now. It’s not just "exercise," it’s literally keeping his arteries from turning into concrete.
Also, the part about unstable plaques? That’s terrifying… but also kind of empowering. Like, I can’t change my genes, but I can change my lunch.
Love that this isn’t just fear-mongering. Real hope here.
Oh please. "You can reverse it?" Really? You think eating kale and taking statins undoes 30 years of fast food and stress? Please. You’re selling snake oil with a side of yoga.
People die from CAD because they’re lazy, not because they didn’t read a Reddit post.
OMG YES THIS!! I just turned 47 and my doc said my calcium score is 890… I was like "wait, I eat avocado toast?!"
Now I’m walking 5k every day, swapped soda for sparkling water, and took my first statin. Still scared, but… kinda proud? 😅
Also, colchicine? I thought that was for gout??
Life is a river, and arteries are its banks. When we pour poison into the river, the banks erode. But if we plant trees-vegetables, movement, peace-the banks grow stronger.
It is not about control. It is about harmony.
🪷
Typical medical propaganda. Statins cause diabetes. Aspirin causes bleeding. PCI is overused. CABG is a scam. Doctors make money off your fear. You’re just parroting pharma ads.
Real solution? Stop eating processed food. That’s it. No pills. No scans. No nonsense.
Wow. So the entire medical establishment is wrong because one guy on the internet says statins are evil? And now we’re supposed to believe that a 30% reduction in heart attacks from colchicine is just "coincidence"?
Oh wait-you’re the guy who thinks vaccines cause autism and that the moon landing was faked. Of course you’d dismiss peer-reviewed science.
Just… stop.
My mom had a heart attack at 52. She didn’t smoke. Didn’t have diabetes. Just worked 60-hour weeks, ate takeout, and never slept.
She’s alive today because she started walking with me after dinner. No fancy meds. Just movement.
It’s not magic. It’s consistency.
And yes, I still nag her about dessert.
Everyone’s focused on the heart. But what about the mind? Chronic stress? Loneliness? Trauma? These are silent killers too.
My aunt had perfect cholesterol. Died at 58 from a sudden blockage. She hadn’t hugged anyone in 12 years.
Love isn’t a supplement. But it might be the best medicine we’re ignoring.
JUST STARTED WALKING 20 MINUTES A DAY AND I FEEL LIKE A NEW PERSON 😍
Also swapped my 3pm candy bar for almonds. No more crash. No more guilt.
My cardiologist cried when she saw my LDL drop 40 points in 3 months. I didn’t even tell her I was crying too. 😭
YOU GOT THIS. YOU’RE NOT ALONE.
Thank you for writing this with such clarity and compassion. Too often, medical information is delivered in a way that feels alienating or overwhelming. This is a rare exception.
I’ve shared this with my entire family, including my teenage niece. She asked if she could start meal-prepping with me. That’s the future right there.
Knowledge, when delivered kindly, is the most powerful intervention we have.
Bro, you really think your 30-min walk is gonna save you? My uncle had a stent and still died 2 years later. You’re not special. Your kale isn’t magic.
Just admit it-your body’s ticking. You’re just delaying the inevitable. Might as well eat the burger.
Just saying.
AMERICA IS THE ONLY COUNTRY THAT HAS THIS PROBLEM BECAUSE WE EAT TOO MUCH SUGAR AND WEAKEN OURSELVES WITH LATTES AND YOGA!
IN RUSSIA, WE DRINK VODKA AND WORK 18 HOURS A DAY-WE DON’T GET HEART DISEASE BECAUSE WE’RE TOUGH!
STOP BEING SOFT.
It is an empirical fact that atherosclerosis is a metabolic disorder, not a vascular one. The lipid hypothesis has been challenged by multiple longitudinal studies, including the Framingham offspring cohort and the PURE study. To reduce CAD to cholesterol levels is a gross oversimplification.
Furthermore, the influence of insulin resistance, gut microbiota, and circadian disruption is not adequately addressed in mainstream guidelines.
One must consider the epigenetic modulation of arterial endothelial function over a lifespan.
my doctor told me i have a 90% blocked artery and i just laughed. like bro i’m 38. i drink monster energy every day. i eat 3 burgers a week. i sleep 4 hours. this is what i signed up for.
if i die, i die. at least i lived.
send help. or send more fries.
Every heart is a story. Every artery, a path walked-sometimes with joy, sometimes with burden.
You don’t need to be perfect. You just need to begin.
One step. One meal. One breath at a time.
Healing is not a destination. It is a daily return to yourself.
And you are worthy of that return.
Always.