For many people with sleep apnea, the CPAP machine is a nightmare - not because it doesn’t work, but because it’s impossible to live with. The mask chafes, the hose tangles, the air pressure feels like a hurricane in your nose, and after a few weeks, most people just give up. That’s where upper airway stimulation comes in. It’s not a mask. It’s not a tube. It’s a tiny device implanted inside your body that wakes up your tongue every time you breathe in - keeping your airway open without you ever having to think about it.
How It Actually Works
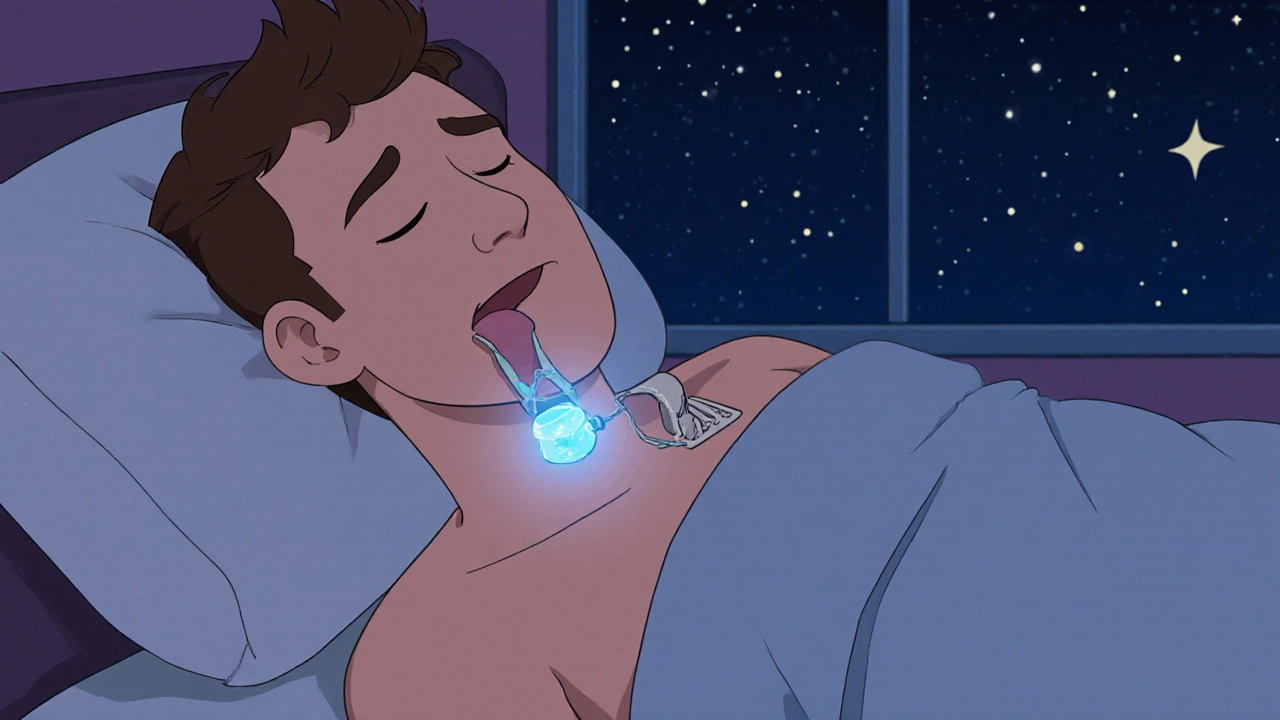
Upper airway stimulation (UAS), most commonly delivered through the Inspire system, doesn’t push air into your nose. Instead, it gently wakes up the nerve that controls your tongue. When you inhale during sleep, the device senses the breath and sends a mild pulse to the hypoglossal nerve. That pulse makes your tongue move forward just enough to stop it from collapsing backward and blocking your throat. It’s like having a silent bodyguard inside your airway, ready to act the moment you need it.
The device has three parts: a small generator (about the size of a pacemaker) implanted under your collarbone, a sensing wire that watches your breathing, and a stimulation wire that wraps around the nerve under your jaw. All of it is placed during a single outpatient surgery - three small incisions, about two to three hours, and you’re home the same day. No overnight stay. No major recovery.
Who Is This For?
This isn’t for everyone. If you’re still trying CPAP and haven’t given up yet, stick with it. UAS is meant for people who’ve tried and failed. The FDA cleared it for adults 22 and older with moderate to severe obstructive sleep apnea - specifically, those with an AHI (apnea-hypopnea index) between 15 and 100 events per hour. You also need a BMI under 35 (or 32 in some cases), and your airway collapse must be mostly in the tongue area, not the soft palate. If your airway shuts completely like a closed door, this won’t help.
Doctors use a special test called drug-induced sleep endoscopy to see exactly where your airway collapses. If your tongue is the main culprit, you’re likely a good candidate. If your soft palate is the problem, you might need something else.
What the Data Shows
The numbers don’t lie. In the STAR trial - the biggest study ever done on this therapy - patients went from an average of 29.3 breathing pauses per hour down to just 9.0 after one year. That’s a 68% drop. Two-thirds of people saw their AHI cut in half or more. And it wasn’t just fewer apneas - people felt better. Less daytime sleepiness. Better focus. More energy.
Long-term data from the ADHERE Registry shows these results hold up for years. Patients with very severe sleep apnea (AHI over 65) still saw big improvements. Even people with higher BMIs (up to 40) benefit now, thanks to a 2023 FDA expansion that widened eligibility.
And here’s the kicker: adherence. CPAP users average about 4 hours a night - if they’re lucky. Inspire users? They wear it nearly every night. Why? Because once it’s implanted, you don’t have to wrestle with straps or clean a humidifier. You just press a button on a small remote before bed. Turn it on. Sleep. Wake up refreshed.

How It Compares to Other Treatments
Let’s be clear: CPAP is still the gold standard. But it’s also the most abandoned treatment in sleep medicine. Studies show 29% to 46% of people quit within the first year. Why? Discomfort. Noise. Claustrophobia. The Inspire system solves all of that.
Compared to surgery like UPPP (removing tonsils and part of the soft palate), UAS is far less invasive. No cutting into your throat. No months of pain. No risk of voice changes or swallowing problems. And unlike UPPP, UAS is reversible. If you ever need to, the device can be removed without leaving permanent damage.
Oral appliances - those mouthpieces that push your jaw forward - work for mild cases. But they’re often ineffective for severe apnea. UAS fills the gap between oral devices and risky surgeries.
Real People, Real Results
On Reddit, someone wrote: "My wife says I’ve stopped snoring completely after two years with Inspire. I feel more rested than I have in decades." That’s not an outlier. Eighty-six percent of users say it’s better than CPAP. Eighty percent recommend it to others. At the Cleveland Clinic, 85% of bed partners reported no snoring or only soft snoring four years after implant.
But it’s not perfect. Some people take a few weeks to adjust to the sensation - a mild tingling or pulling in the tongue. A small number report temporary tongue weakness. About 2% get minor infections at the incision sites. And yes, you have to remember to turn it on every night. If you forget, it won’t work. But most users say that’s a small price to pay for a full night’s sleep without a mask.

The Process: From Diagnosis to Implant
Getting started isn’t quick. First, you need a sleep study confirming moderate to severe OSA. Then, you must have tried CPAP for at least three months and documented that you couldn’t tolerate it. After that, you’ll have a sleep endoscopy - a short procedure where you’re put under light sedation and a camera looks inside your throat to see where your airway collapses.
If you qualify, the surgery is scheduled. It’s done under general anesthesia. Most people go home the same day. Recovery? Usually five to seven days. You’ll have some soreness in your neck and chest, but nothing like major surgery.
One month after implant, your doctor turns the device on. They’ll adjust the stimulation level over several visits - usually at 1, 3, 6, and 12 months - until it’s just right for you. You’ll get a remote control. That’s your key to sleep. Press it before bed. Press it again when you wake up. Simple.
Cost and Coverage
Yes, it’s expensive. The total cost - device, surgery, hospital fees - runs between $35,000 and $40,000. But here’s what most people don’t realize: over 10 years, that’s roughly what you’d spend on CPAP machines, masks, filters, humidifiers, and doctor visits. And that’s not counting lost productivity, missed work, or health complications from untreated sleep apnea.
Good news: insurance covers it. Medicare pays for it in 95% of cases. Most private insurers do too. The American Academy of Sleep Medicine officially recommends UAS as a treatment option for CPAP-intolerant patients. That means your doctor can get pre-approval without fighting a battle.
What’s Next?
The technology is still evolving. Newer versions are smaller. Some are being tested to work without a sensing wire. AI is being used to predict who will respond best - based on the shape of their airway, not just their BMI or AHI. The market is growing fast. Over 200,000 people worldwide have had the device implanted. That number is expected to double by 2028.
For people who’ve spent years lying awake, exhausted, and frustrated - this isn’t just another treatment. It’s a return to normal life. To sleeping next to your partner without guilt. To driving without nodding off. To waking up and actually feeling like you’ve rested.
If you’ve tried CPAP and quit - if you’ve accepted that snoring and fatigue are just part of life - this might be the answer you didn’t know existed. It’s not magic. But it’s real. And for the right person, it changes everything.
Is upper airway stimulation the same as a pacemaker?
It’s similar in size and placement - the generator is implanted under the collarbone like a pacemaker - but it doesn’t regulate your heartbeat. Instead, it stimulates the nerve that controls your tongue to keep your airway open during sleep. It’s a sleep therapy device, not a cardiac one.
Can I have an MRI after getting the implant?
Yes, but only under specific conditions. The Inspire device is MRI-conditional, meaning you can have an MRI of your head or neck if the machine is set to certain safety limits and the device is turned off. Full-body MRIs are not allowed. Always inform your radiology team you have an implanted stimulator before any scan.
Does it help with snoring?
Yes - and that’s one of the most immediate benefits. Since snoring is caused by airway collapse, keeping the airway open stops the vibrations that cause it. Studies show 85% of bed partners report no snoring or only soft snoring after four years of use.
How long does the battery last?
The generator’s battery lasts about 8 to 11 years, depending on usage. When it runs low, you’ll get a warning from your doctor. Replacing it is a minor surgery - similar to replacing a pacemaker battery. The leads don’t need to be replaced unless there’s a problem.
Will I feel the device when I’m awake?
No. The stimulation only happens during sleep, when you’re breathing in. When you’re awake, the device is inactive. Some people feel a slight tingling in their tongue when the device is first turned on, but that usually fades within a few weeks as the nerves adjust.
Can I travel with the device?
Absolutely. The remote control works like a TV remote - no Wi-Fi or Bluetooth needed. You can fly, drive, or go camping. Airport security won’t set off alarms, but you may be asked to show your patient ID card (which you’ll receive after implant). It’s a good idea to carry it with you.
Is this covered by insurance in the UK?
As of 2025, upper airway stimulation is available in the UK through the NHS in select specialist sleep centers, but access is limited. Most patients pay privately or through private insurance. The cost is similar to the US - around £25,000 to £30,000 - but clinical guidelines now recognize it as a viable option for CPAP-intolerant patients.
What happens if I gain weight after the implant?
Weight gain can reduce the effectiveness of any sleep apnea treatment, including UAS. If your BMI rises above 35, your apnea may return. The device can be re-titrated (adjusted) to increase stimulation, but if your airway narrows too much from fat deposits, the therapy may not work as well. Maintaining a healthy weight is still important.
Can children get this implant?
No. The FDA and other regulatory bodies have only approved UAS for adults 22 and older. Children with sleep apnea are treated with tonsillectomy, orthodontic devices, or CPAP. This therapy is not designed or tested for younger patients.
Are there alternatives to Inspire?
Inspire is the only FDA-approved upper airway stimulation system currently on the market. Other companies are developing similar devices, but none are widely available yet. For now, Inspire is the only option for nerve-stimulating therapy for sleep apnea.




One comment
this thing sounds like magic but i just want to sleep without feeling like i'm wearing a space helmet on my face
Oh great. Another overhyped tech solution for people who can't be bothered to lose 10 pounds or sleep on their side. We've got a whole industry built on making lazy people feel better about their bad habits.
I've seen this technology change lives in my sleep clinic. People who hadn't slept through the night in 15 years are now playing with their grandkids without napping at 3 p.m. It's not a cure-all, but for the right person, it's a revolution. The data is solid, the safety profile is strong, and the adherence rates speak louder than any skeptic's cynicism.
Of course it works. Because nothing says American healthcare like slapping a $40k implant into someone's neck because they refused to use a $100 machine. Meanwhile, in Germany, they just tell you to stop eating nachos before bed. Guess which approach is cheaper?
I had CPAP for two years. I hated it. I felt like a robot. I felt like a failure. Then I got the Inspire. The first night I slept without waking up gasping, I cried. Not because I was sad. Because I finally felt human again. This isn't about money. It's about dignity.
The key thing people miss is that UAS isn't replacing CPAP it's replacing abandonment. The real failure isn't the machine it's the system that doesn't offer alternatives. Most patients aren't lazy they're desperate. They've tried everything. They've worn the mask until their face was raw. They've sat in the dark for hours because the noise kept them awake. UAS isn't a luxury it's the last option that actually works. And the fact that insurance covers it means we're finally treating sleep apnea like the life-threatening condition it is
Let's not ignore the 2% infection rate. Or the fact that the device can migrate. Or that long-term nerve stimulation effects are still unknown. And let's not pretend this isn't a profit-driven industry pushing a high-margin product. The data looks good but it's all industry-funded. Where are the independent, long-term studies?
So you're telling me I should spend $40k so I don't have to clean a hose? That's not a medical breakthrough. That's a glorified vibrator for your tongue. I've got a cousin who got this done and now he can't even swallow soup without feeling like his tongue is being pulled. You call that progress?
I am from India and here this is not available yet but i read about it and i think it is beautiful that someone figured out how to help people sleep without masks. In my village people still use wet towels on their forehead to stay cool at night and no one talks about sleep apnea. This is science that sees the person not just the symptom
I used to think this was a scam until my wife told me I stopped snoring so hard the dog stopped barking at night. I used to wake up with my throat on fire. Now I wake up and actually remember my dreams. I don't care if it costs $40k. I care that I can now hold my daughter without feeling like I'm going to pass out. This isn't about technology. This is about being there. For your family. For yourself. For the first time in decades.