Upper Airway Stimulation: What It Is, Who It Helps, and What You Need to Know
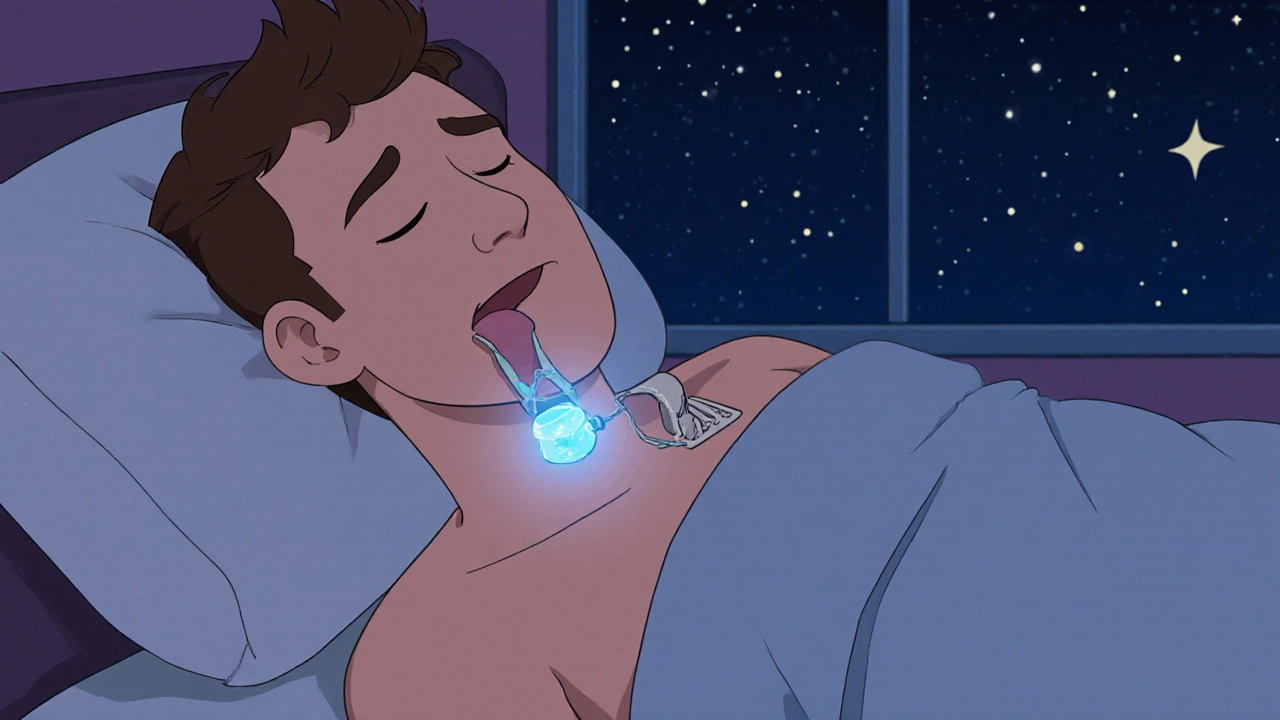
When you hear upper airway stimulation, a medical device that gently activates the nerve controlling tongue movement during sleep to keep the airway open. Also known as hypoglossal nerve stimulation, it's not a cure—but for many, it’s the first real relief after years of struggling with CPAP masks, noisy machines, and endless fatigue. This isn’t science fiction. It’s an FDA-approved implant, roughly the size of a pacemaker, that watches your breathing and wakes up your tongue just enough to stop it from blocking your airway at night.
It’s not for everyone. If you’re overweight, have severe lung disease, or can’t tolerate even mild anesthesia, it’s probably not right for you. But if you’ve tried CPAP and quit because it felt like wearing a helmet while sleeping, or if your doctor says you’re a good candidate, this could change your life. People who use it report fewer apnea events, better sleep quality, and less daytime grogginess—often without the bulk of a mask. The device is implanted under the skin in your chest, with a lead running to the nerve under your jaw. It turns on automatically when you fall asleep and shuts off when you wake up. No buttons. No tubes. Just quiet, uninterrupted rest.
It works best for people with moderate to severe obstructive sleep apnea who aren’t helped by weight loss or position changes. Studies show about 70% of users see a 50% or better drop in breathing interruptions. That’s the same improvement most people get from CPAP—but without the noise, the skin sores, or the feeling of being tethered to a machine. And unlike surgery that removes tissue, this is reversible. If it doesn’t work, you can have it removed.
What you won’t find in most ads is how expensive it is. Insurance covers it for qualifying patients, but getting approval can take months. You’ll need a sleep study, a doctor’s note, and often proof you’ve tried and failed with CPAP. Some people spend over a year jumping through hoops just to get the green light. But for those who make it through, the payoff is real: waking up without a headache, feeling alert in the afternoon, and actually sleeping through the night without your partner nudging you.
It’s not the only option. There are oral appliances, nasal devices, and even newer procedures that shrink the soft palate. But for people who need something more reliable than a mouthguard and less intrusive than a tonsillectomy, upper airway stimulation stands out. It’s the middle ground between a mask and major surgery—and for many, it’s the only thing that finally works.
Below, you’ll find real stories and practical advice from people who’ve walked this path. From how to prepare for the implant to what to expect during recovery, from insurance battles to life after the device turns on—you’ll find answers here. No fluff. No hype. Just what matters when your sleep is on the line.