When your doctor prescribes Indomethacin (brand name Indocin), you probably wonder how it measures up against the other non‑steroidal anti‑inflammatory drugs (NSAIDs) on the market. This guide breaks down the most relevant differences-efficacy, safety, dosing, cost, and typical uses-so you can decide whether Indocin is the best fit for your condition or if another NSAID might serve you better.
Key Takeaways
- Indomethacin is the most potent anti‑inflammatory among common NSAIDs, making it ideal for severe arthritis and gout.
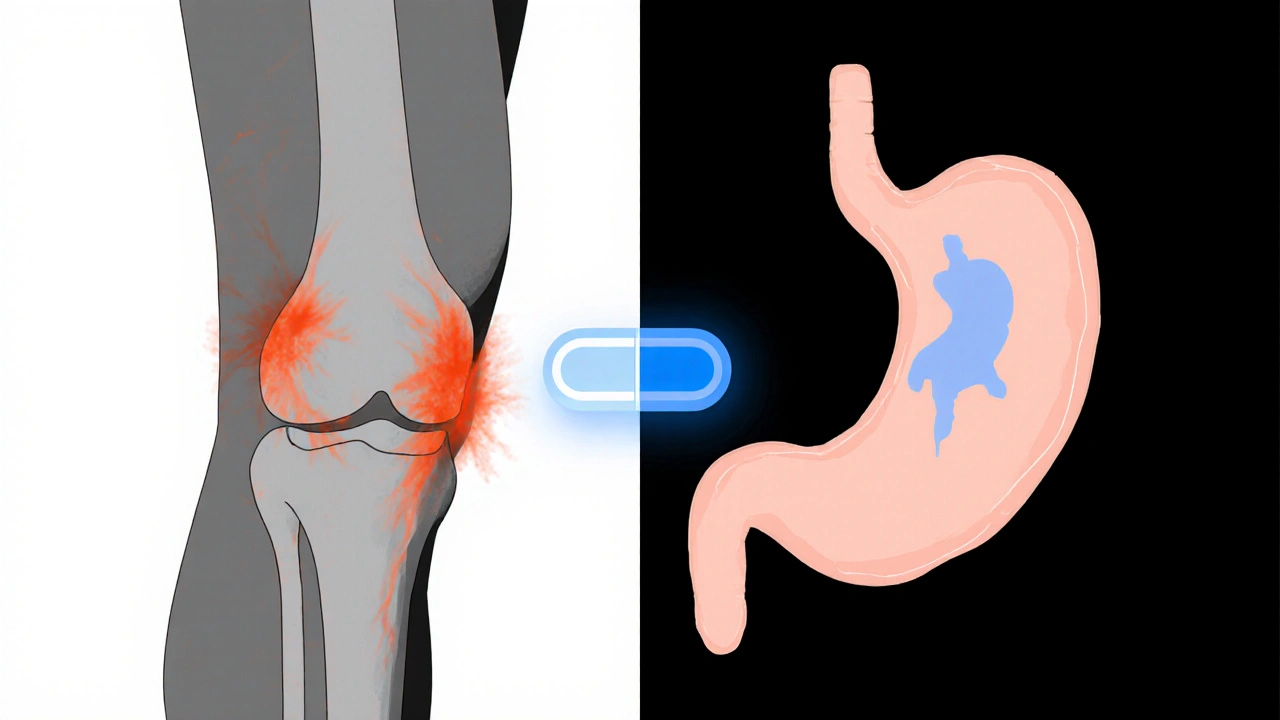
- Its gastrointestinal (GI) and cardiovascular risk profile is higher than newer, COX‑2‑selective options like celecoxib.
- Cost varies widely; generic indomethacin is affordable, but some alternatives (e.g., naproxen) may be cheaper in large‑quantity packs.
- Kidney‑friendly patients often prefer meloxicam or ibuprofen at the lowest effective dose.
- Choosing the right NSAID hinges on your specific diagnosis, comorbidities, and how you respond to side‑effects.
What Is Indomethacin?
Indomethacin is a non‑steroidal anti‑inflammatory drug first approved in 1963. It works by inhibiting cyclooxygenase (COX‑1 and COX‑2) enzymes, which reduces prostaglandin production and therefore pain, swelling, and fever. Typical oral doses range from 25mg to 75mg two to three times a day, depending on the condition.
Indomethacin shines in treating gout flares, ankylosing spondylitis, and certain forms of osteoarthritis where strong inflammation control is needed. However, its potency comes with a higher chance of stomach irritation, ulcers, and a modest increase in cardiovascular events.
How We Compare NSAIDs
To give you a clear picture, we evaluated each drug on five practical criteria:
- Anti‑inflammatory strength - How well it reduces swelling and pain.
- GI safety - Risk of ulcers, bleeding, or dyspepsia.
- Cardiovascular risk - Impact on blood pressure, heart attacks, and strokes.
- Dosing convenience - Frequency and need for dose adjustments.
- Cost & accessibility - Price per defined daily dose and availability of generics.
We then matched each drug against common patient scenarios to see which one usually comes out on top.
Alternative NSAIDs at a Glance
Below are the main contenders we’ll compare with Indomethacin.
Naproxen is a longer‑acting NSAID commonly used for arthritis and musculoskeletal pain. Its standard dose is 250mg to 500mg twice daily.
Ibuprofen is the most widely used OTC NSAID, taken at 200mg to 400mg every 4-6hours for mild‑to‑moderate pain.
Celecoxib is a COX‑2‑selective drug that aims to spare the stomach. The usual prescription dose is 100mg once or twice daily.
Meloxicam provides a once‑daily dosing option (7.5mg to 15mg) and has a slightly lower GI risk than non‑selective NSAIDs.
Diclofenac is popular for acute pain and sports injuries, often prescribed at 50mg three times daily.
Side‑Effect Profiles Compared
| Drug | Anti‑inflammatory rank* (1=strongest) | GI ulcer risk | Cardiovascular risk | Dosing frequency | Typical cost (UK, per month) |
|---|---|---|---|---|---|
| Indomethacin | 1 | High | Moderate | 2-3×day | £5-£12 |
| Naproxen | 2 | Medium‑High | Low‑to‑moderate | 2×day | £4-£9 |
| Ibuprofen | 3 | Medium | Low | 3-4×day (OTC) / 2×day (prescribed) | £2-£7 |
| Celecoxib | 2 | Low | High (especially with hypertension) | 1-2×day | £12-£25 |
| Meloxicam | 3 | Low‑Medium | Low‑to‑moderate | once daily | £6-£15 |
| Diclofenac | 2 | Medium | High (especially with existing heart disease) | 2-3×day | £5-£13 |
*Ranking is based on clinical studies measuring reduction in joint swelling and pain scores.
When Indomethacin Is the Best Choice
- Severe gout attacks - Its rapid, strong anti‑inflammatory action often shortens flare‑ups within 24-48hours.
- Ankylosing spondylitis - Patients needing high‑dose therapy benefit from the potency of indomethacin.
- Patients without major GI or heart risk - If you have a healthy stomach lining and no history of hypertension, indomethacin’s benefits may outweigh its risks.
Because the drug is usually taken multiple times a day, strict adherence is crucial. Missing doses can cause rebound inflammation and may lead to a flare‑up.
Scenarios Favoring Alternative NSAIDs
Naproxen is often preferred for chronic arthritis when patients need a balance of efficacy and lower cardiovascular risk. Its twice‑daily schedule is easier than indomethacin’s three‑times‑daily regimen.
Ibuprofen is the go‑to for mild‑to‑moderate pain, especially when an over‑the‑counter option is desired. It’s gentler on the stomach than indomethacin but less potent for deep joint inflammation.
Celecoxib works well for patients with a history of ulcers who still need strong pain relief. However, if you have high blood pressure or heart disease, discuss the elevated cardiovascular risk with your doctor.
Meloxicam offers once‑daily dosing, which improves compliance for older adults. Its GI risk sits between ibuprofen and indomethacin, making it a middle‑ground choice.
Diclofenac is frequently used for sports injuries and acute musculoskeletal pain because it takes effect quickly. Yet, due to its higher cardiovascular danger, it’s generally avoided in patients with existing heart conditions.

Practical Tips for Using Indomethacin Safely
- Take the medication with food or a full glass of milk to lessen stomach irritation.
- Avoid alcohol and concurrent use of other NSAIDs, as the combination dramatically raises ulcer risk.
- If you’re on blood thinners (e.g., warfarin), monitor your INR more closely; indomethacin can increase bleeding tendency.
- Stay hydrated and monitor kidney function if you have diabetes or mild renal impairment.
- Schedule a follow‑up blood test after 2-4weeks to check liver enzymes and kidney markers.
How to Talk to Your Doctor About Switching NSAIDs
Bring a concise list of your current meds, any known allergies, and a brief description of your pain pattern. Ask direct questions such as:
- “Given my ulcer history, is indomethacin safe for me?”
- “Would a COX‑2‑selective drug lower my GI risk?”
- “If I need to take it long‑term, how often should we check my blood work?”
Doctors appreciate patients who are informed but also realistic about potential side‑effects. Sharing previous experiences with OTC NSAIDs can guide them toward a tailored regimen.
Frequently Asked Questions
Can I take indomethacin with a proton‑pump inhibitor (PPI)?
Yes, combining indomethacin with a PPI like omeprazole can reduce the chance of stomach ulcers. However, the protection isn’t absolute, so still monitor for any GI symptoms.
Is indomethacin safe during pregnancy?
Indomethacin is classified as a Category C drug in the UK, meaning it should be avoided especially in the third trimester because it may affect fetal kidney function and close the ductus arteriosus.
How long can I stay on indomethacin?
Short‑term use (a few weeks) is generally safe for acute flares. For chronic conditions, doctors usually rotate to a less aggressive NSAID after 3months to limit GI and renal complications.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed dose-don’t double up, as that raises the risk of stomach irritation.
Can indomethacin interact with antihypertensive drugs?
Yes. Indomethacin can blunt the effect of ACE inhibitors and diuretics, potentially raising blood pressure. Monitoring and dose adjustments may be needed.
Choosing the right NSAID is a balance of potency, safety, and convenience. Indomethacin remains a heavyweight for severe inflammation, but newer agents or more gentle options may be a smarter fit for everyday pain management. Always discuss your full medical picture with a healthcare professional before starting or switching any medication.





One comment
When you dig into the pharmacology of NSAIDs you quickly discover that indomethacin isn’t just another over‑the‑counter painkiller, it’s a molecule with a very specific affinity for both COX‑1 and COX‑2 enzymes, which explains its reputation as the most potent anti‑inflammatory in the class. Its mechanism of action translates into rapid reduction of prostaglandin synthesis, making it especially effective for gout flares and ankylosing spondylitis where the inflammatory burden is high. Because it blocks COX‑1 as well as COX‑2, the gastric mucosa loses one of its primary defensive pathways, which is why the gastrointestinal risk profile is markedly higher than that of more selective agents like celecoxib. In real‑world practice you’ll often see clinicians pairing indomethacin with a proton‑pump inhibitor to mitigate ulcer formation, but even that combination does not eliminate the danger entirely. The drug’s half‑life is relatively short, necessitating multiple daily doses – usually two to three times a day – which can be a compliance challenge for many patients. Cost‑wise, generic indomethacin is inexpensive, typically ranging from five to twelve pounds per month in the UK, yet the hidden costs of monitoring labs and managing side effects can add up. For patients with a history of cardiovascular disease, the moderate risk associated with indomethacin may tip the balance in favor of a COX‑2‑selective alternative, especially if they are already on antihypertensive therapy. Renal considerations are also important; indomethacin can reduce renal blood flow, so those with chronic kidney disease need close monitoring of creatinine and electrolytes. The drug’s potency means that dose titration must be done carefully – starting low and adjusting based on therapeutic response and side‑effect tolerance is the safest strategy. In terms of drug–drug interactions, indomethacin can blunt the antihypertensive effects of ACE inhibitors and diuretics, and it can increase the bleeding risk when combined with anticoagulants like warfarin. While it is a heavyweight in the NSAID arena, it is not without its rivals: naproxen offers a comparable anti‑inflammatory effect with a somewhat better cardiovascular profile, ibuprofen is more convenient for mild pain but less effective for severe inflammation, and meloxicam provides once‑daily dosing which improves adherence for older adults. Ultimately, the decision to use indomethacin should be individualized, taking into account the severity of inflammation, the patient’s comorbid conditions, and their ability to adhere to a multi‑dose regimen. If you fall into the category of severe gout or ankylosing spondylitis with a relatively clean gastrointestinal and cardiovascular history, indomethacin may be the most logical choice. Conversely, if you are juggling multiple chronic illnesses or have a history of ulcers, a gentler NSAID or a COX‑2‑selective agent might serve you better. Always have a candid discussion with your healthcare provider about the risk–benefit calculus before committing to long‑term therapy.
One might contemplate the ethical dimension of prescribing a drug whose efficacy is counterbalanced by tangible risk, and in doing so, we encounter the perennial medical paradox of benefit versus harm. Indomethacin, in its robust anti‑inflammatory capacity, epitomizes this dichotomy, offering swift amelioration of severe pain while simultaneously jeopardizing gastrointestinal integrity. From a pharmacological standpoint, its non‑selective inhibition of cyclooxygenase enzymes is both its strength and its Achilles’ heel. The clinician, therefore, bears a fiduciary responsibility to weigh these attributes against the patient’s individual risk profile. In practical terms, this translates to meticulous assessment of comorbidities, vigilant monitoring, and, when appropriate, the adjunctive use of gastroprotective agents.
Looking at the data tables for NSAID adverse events, indomethacin consistently shows higher rates of GI complications compared with naproxen or ibuprofen, which suggests a need for stricter patient selection. The statistical significance is clear, yet many prescribers overlook it in favor of raw potency. From an analytical perspective, the cost‑benefit ratio tilts unfavorably unless the inflammatory condition is truly refractory. It would be prudent to incorporate regular endoscopic screening for at‑risk patients if long‑term therapy is considered.
i think it's cool how u can still use indocin if u watch ur stomach
Everyone has diff needs when it comes to pain meds we all feel the same need to get relief but each drug has its own vibe juggling effectiveness and safety is key
Indeed, a balanced approach is paramount; by aligning therapeutic goals with individual risk factors, clinicians can tailor NSAID therapy to optimise outcomes while minimising adverse events.
Yo, if you’re crunching the PK/PD curves, you’ll see indomethacin's Tmax hits around 2‑4 hours and its Cmax is pretty high, which is why you feel that rapid drop in inflammatory cytokines. But remember, the therapeutic window is narrow – overshoot and you’re courting GI bleed territory. So load it with a PPI, watch renal labs, and keep dose titration tight. For anyone in sports rehab, you might prefer diclofenac for quick onset, but don’t forget the cardio red flag.
Great points, Michael! Keeping an eye on labs while leveraging the fast action of indomethacin can really make a difference for patients battling acute flares 😊.
While the lay discourse often romanticises over‑the‑counter remedies, a discerning clinician recognises that indomethacin occupies a niche reserved for the most recalcitrant inflammatory pathologies, thereby warranting its elevated status in the pharmacopeia.
Honestly this whole conversation about indomethacin feels like a never ending saga of risk versus reward the way you just laid out the stats and the mechanisms is impressive but also a bit overwhelming for the average reader the thing about the GI bleeding rates especially when you factor in age related mucosal vulnerability is something that cannot be ignored but at the same time the potency for gout attacks is unmatched and that is why many rheumatologists will still reach for indocin in severe cases the nuance here is that you need a comprehensive monitoring plan including regular H pylori testing and possibly a scheduled endoscopy for chronic users and let’s not forget about the drug interactions with antihypertensives which can blunt their effect leading to uncontrolled blood pressure which is a whole other can of worms for patients with comorbid hypertension finally I think the key takeaway is that indomethacin is not a one size fits all solution and must be prescribed with the utmost caution and patient education for safe use
Thank you for highlighting these considerations; a patient‑centred dialogue that incorporates thorough risk assessment and clear instructions on gastroprotective strategies is essential for safe indomethacin utilisation.
You know the pharma giants don’t want you to hear about the real side effects they’re hiding in the fine print they push these drugs on us while they keep the money rolling in and the watchdogs stay silent
In the grand tapestry of analgesic therapeutics, indomethacin represents a formidable but precarious thread, demanding scholarly prudence from its custodians.
Interesting take, I’ve seen both sides and it really comes down to personal health history.
The reality is that many patients ignore the subtle warnings and dive straight into potent NSAIDs like indomethacin without proper counseling, leading to preventable complications that could have been avoided with better education.