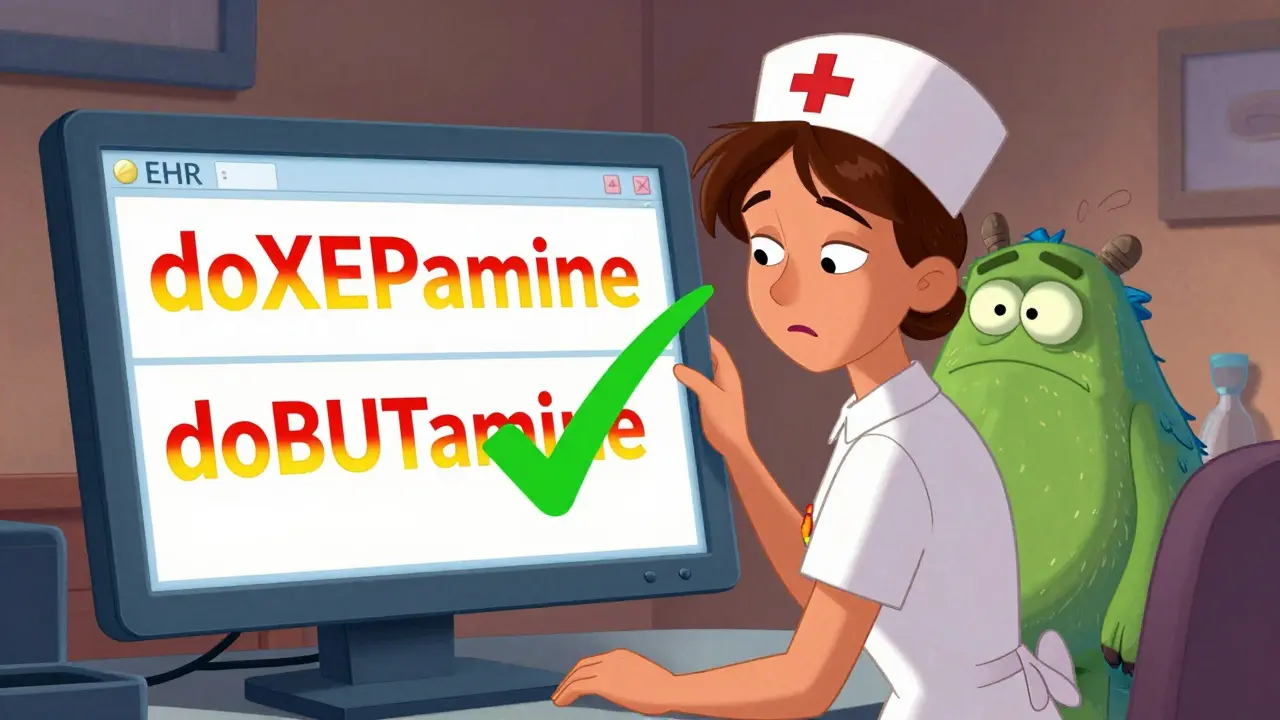
Every year, thousands of people in the U.S. and UK are harmed because two drug names look or sound too similar. One pill can be mistaken for another - hydroCODONE for hydroHYDRAZINE, doXEPamine for doBUTamine - and the results aren’t just inconvenient. They’re deadly. If you’re a pharmacist, nurse, or even a patient double-checking your own meds, knowing how to spot these look-alike names isn’t optional. It’s life-saving.
Why Look-Alike Names Are So Dangerous
It’s not just about bad handwriting or rushed prescriptions. The problem runs deep. Over 3,000 drug name pairs are flagged as look-alike or sound-alike (LASA) by the U.S. Pharmacopeial Convention. These aren’t random typos. They’re names that share 60-80% of their letters or syllables. That’s enough to trick even experienced staff. A 2006 study found that 1.7 errors happen per 1,000 prescriptions. Worse, 34% of those errors reach the patient. And 7% cause real harm - falls, organ damage, even death. The FDA started its Name Differentiation Project back in 2001 because the numbers were climbing. By 2023, they’d reviewed over 1,800 drug names and officially recommended tall man lettering (TML) for 35 high-risk pairs. That’s not just a suggestion. It’s now part of the standard of care.What Is Tall Man Lettering (TML)?
Tall man lettering is simple in theory but powerful in practice. It uses uppercase letters to highlight the parts of drug names that differ. For example:- hydrOXYzine vs. hydrALazine
- vinBLAstine vs. vinCRIStine
- CISplatin vs. CARBOplatin
How to Spot Look-Alike Names in Real Life
You won’t always have a computer system warning you. Sometimes, you’re looking at a handwritten script, a faded label, or a crowded pharmacy shelf. Here’s how to protect yourself:- Read the full name out loud. Say it slowly. Does it sound like another drug you know? Try saying “Hydroxyzine” and “Hydralazine” out loud. The difference is subtle - but real.
- Check for tall man lettering. Look at every label - electronic, printed, or handwritten. If you don’t see capital letters in the middle of the name, ask why. It’s not standard unless it’s a known LASA pair.
- Compare brand and generic names. Valtrex (valacyclovir) and Valcyte (valganciclovir) are both antivirals. Seeing both names together helps you remember: “Valtrex is for herpes, Valcyte is for CMV.” Purpose matters.
- Verify with the prescription intent. If a patient is on insulin, and the label says “Humalog,” double-check it’s not “Humulin.” Ask: “Is this for rapid-acting or long-acting control?” The reason for the drug helps confirm you’ve got the right one.
- Use the 3-step rule. Read the label when you pick it up. Read it again when you hand it off. Read it one more time before giving it to the patient. That simple habit cuts errors by over half.
Technology Can Help - But Only If It’s Set Up Right
EHR systems and pharmacy software should be doing the heavy lifting. But many aren’t configured properly.- Drug names should never appear consecutively in dropdown menus. If “Hydroxyzine” and “Hydralazine” are right next to each other, someone’s going to click the wrong one.
- Searches should require at least 5 letters before showing results. This cuts down on overwhelming lists and reduces selection errors by 68%.
- Alerts should only trigger for high-risk pairs. Too many alerts, and clinicians start ignoring them. One study found 49% of LASA alerts were overridden.
The Big Problem: Inconsistent Implementation
The biggest threat isn’t the names themselves - it’s inconsistency. A nurse in an ICU forum shared this: “The EHR shows hydroCODONE with tall man letters, but the MAR doesn’t. I get confused switching between systems.” That’s not rare. A 2022 survey of over 1,200 pharmacists found that 65% saw TML applied inconsistently across systems. And 42% said it was often missing from handwritten orders. Handwritten prescriptions are still a major source of LASA errors. Forty-one percent of reported mistakes come from them. Even if the doctor writes “hydroCODONE,” the pharmacy might print it as “hydrocodone” - and the warning is gone. And it’s not just about letters. Poor printing, low contrast, small fonts - all of it makes TML useless. The Joint Commission requires a minimum 12-point font and 4.5:1 color contrast for labels. If your printer is fading or the label is printed on a colored background, you’re risking patient safety.What’s Working: Real Success Stories
Johns Hopkins Hospital reduced LASA errors by 67% over two years. How? They didn’t just use TML. They added three things:- Mandatory purpose-of-treatment notes on every prescription.
- Computer alerts only for the highest-risk pairs.
- Staff training with real-world case studies.

What You Can Do Right Now
You don’t need a $150,000 system to make a difference. Start here:- Always read the full drug name. Never skim. Even if you’ve seen it a hundred times.
- Ask: “Is this tall man lettered?” If not, question it.
- Use the 3-step verification. Read it. Read it again. Read it once more.
- Report inconsistencies. If the EHR and the label don’t match, tell your supervisor. Document it.
- Train new staff. Show them the list of common LASA pairs. Make it part of onboarding.
The Future Is Here - But Only If We Use It
New tools are coming. AI models like Google Health’s Med-PaLM 2 can predict confusion with 89% accuracy. Smartphone apps can scan pill bottles and flag look-alikes. The National Council for Prescription Drug Programs just released a new standard that lets EHRs, pharmacies, and supply chains talk to each other in real time about LASA risks. But none of it matters if we rely on tech alone. Dr. Michael Cohen of ISMP says it best: “Tall man lettering is necessary but not sufficient.” The truth is, no system is foolproof. People still make mistakes under pressure. Fatigue, distractions, time crunches - they all play a role. That’s why the most effective defense is still a trained, alert, and cautious human. You’re not just checking a name. You’re checking a life.What to Do If You Spot a Look-Alike Error
If you catch a mistake - even a near-miss - report it. Don’t assume someone else will. Most hospitals have a safety reporting system. Use it. These reports help update the FDA’s list and improve systems for everyone. Don’t wait for someone to get hurt. If you see a label without tall man lettering on a high-risk pair, speak up. If you see two similar names next to each other on a screen, flag it. If a handwritten script looks ambiguous, call the prescriber. That call might save a life.What are the most common look-alike drug name pairs?
The FDA’s current list of 35 high-risk pairs includes: hydroCODONE vs. hydroHYDRAZINE, doXEPamine vs. doBUTamine, vinBLAStine vs. vinCRIStine, CISplatin vs. CARBOplatin, and hydrOXYzine vs. hydrALAzine. These are the most frequently confused. Insulin names like Humalog and Humulin are also high-risk. Always check the official FDA TML list for updates.
Is tall man lettering required by law?
It’s not federally mandated by law, but it’s required under the Joint Commission’s National Patient Safety Goal NPSG.01.01.01, which applies to all accredited U.S. healthcare organizations. Failure to comply can result in loss of accreditation. Most hospitals treat it as mandatory.
Can I rely on computer alerts to catch look-alike errors?
No. Computer alerts catch about 76% of potential errors, but clinicians override nearly half of them due to alert fatigue. TML and verification habits are still your best defense. Alerts should support, not replace, human judgment.
Why don’t all pharmacies use tall man lettering?
Some use outdated software that doesn’t support it. Others print labels on low-quality printers that fade capital letters. Handwritten prescriptions often skip it entirely. Inconsistent implementation is the biggest barrier - not lack of awareness.
How can patients protect themselves from look-alike drug errors?
Patients should always read the label on their medication bottle. Ask the pharmacist: “Is this the right drug for my condition?” and “Does this name look like any other medicine I take?” If the name doesn’t have capitalized letters in the middle, ask why. Don’t assume it’s correct just because it came from the pharmacy.




One comment
Been working in a pharmacy in Mumbai for 8 years, and I can tell you - this isn't just a US problem. We get mix-ups all the time with insulin names and antibiotics. Tall man lettering? We don’t even have it on half our labels. But we do read everything out loud - and we ask the patient to repeat it back. Simple, but it works.
Also, patients here often don’t know their meds’ generic names. So we write them in Hindi too. Little thing, big difference.
OMG YES. I had a nurse hand me a vial of hydralazine thinking it was hydroxyzine last month. I nearly threw up. I didn’t even know this was a thing until I googled it after. Now I screenshot the FDA list and keep it on my phone. Like, literally. Don’t trust your brain. Trust the damn capitals.
As a clinical pharmacist, I’ve reviewed over 200 LASA-related incidents in our EHR logs. The data is clear: TML reduces visual confusion by 30–40% when implemented consistently. But the real killer is inconsistent application - EHR vs. printed label vs. barcode system. We had a near-miss last quarter because the Pyxis machine defaulted to lowercase, while the CPOE used TML. That’s not a tech failure. That’s a policy failure.
Also, don’t forget: 78% of errors occur during shift changes. Fatigue + distraction + inconsistent formatting = perfect storm.
so like… we’re spending 150k on scanners but still letting doctors scribble ‘hydralazin’ on a napkin? and we’re surprised people die?
also, tall man lettering is basically just yelling at the drug name. like… why not just call it ‘HYDROXYZINE’ and be done with it? but nooo, we gotta make it ‘hydrOXYzine’ like it’s a secret code only pharmacists can decode. genius.
THIS IS WHY PEOPLE DIE. YOU THINK YOU’RE BEING CAREFUL? YOU’RE NOT. I SAW A NURSE GIVE A PATIENT HUMALOG INSTEAD OF HUMULIN. THE PATIENT WENT INTO HYPOGLYCEMIC SHOCK. SHE SAID ‘I THOUGHT THEY WERE THE SAME.’
NO THEY’RE NOT. AND IF YOU’RE TOO LAZY TO READ THE FULL NAME, YOU DON’T DESERVE TO WORK IN HEALTHCARE. THE FDA LIST IS PUBLIC. THE JOINT COMMISSION REQUIRES IT. YOU’RE NOT A CAREGIVER - YOU’RE A LIABILITY.
Why do we even care? If the patient dies, the hospital gets sued. If they live, they get a new prescription. The system works. Let the lawyers handle it.
Just wanted to say thank you for writing this. I’m a new RN and I had no idea about LASA pairs until I read this. I printed the FDA list and taped it to my locker. Also, I started doing the 3-step rule with every med I give - even if it’s something I’ve given 100 times. I used to think I was being slow. Now I know I’m being safe. 💙
Also - if you’re a manager reading this: please, please, please fix the label printer in Unit 3B. The ‘O’ in hydroCODONE is barely visible. I almost missed it yesterday.
Let’s be real - this whole TML thing is just a band-aid on a hemorrhage. We’re treating symptoms, not the disease. The disease is that we allow 1,800+ drug names to be approved with near-identical spellings in the first place. Why not just have a centralized naming authority? Why not ban any name that shares more than 50% of its syllables with an existing drug? Why are we letting pharmaceutical companies name drugs like they’re naming their pets? ‘Hydroxyzine’? ‘Hydralazine’? Who thought that was a good idea? Someone got paid for this? Someone got a bonus?
We’ve got AI that can predict stock trends and generate poetry - but we can’t stop a pharmacy from giving someone a lethal dose because two names look like twins separated at birth? This isn’t healthcare. This is a bad sitcom written by a drunk copywriter.
Oh, the noble quest to distinguish between hydroCODONE and hydroHYDRAZINE. How quaint. I suppose next we’ll be legislating the difference between ‘citalopram’ and ‘citapram’. I mean, really - if you can’t tell the difference between two words that differ by two letters, perhaps you shouldn’t be entrusted with human lives. Or maybe, just maybe, the problem isn’t the names - it’s the people reading them.
Also, tall man lettering? Sounds like something a Victorian librarian would do to mark forbidden texts. How very… British.
Barcoding reduces errors by 80%? That’s the claim. But in real-world settings, compliance is under 60%. And when you factor in workflow disruptions, staff resistance, and downtime, the net benefit is negligible. TML is more cost-effective. Also, most LASA errors occur during transcription - not dispensing. So your ‘gold standard’ is misaligned with the actual failure point.
Here in Nigeria, we don’t have EHRs or barcode scanners. We use paper and our eyes. And we still don’t have many mix-ups. Why? Because we talk to the patient. We ask: ‘What is this for?’ If they say ‘for high blood’, and the drug is hydroxyzine - we know it’s wrong. We don’t need fancy letters. We need people who care.
Look, I’ve been in this game for 20 years and I’ve seen everything. You think TML is the answer? Nah. The real issue is that nurses are overworked and underpaid. They’re doing 12-hour shifts, skipping lunch, and getting 3 minutes to verify 20 meds. No amount of capital letters will fix that. The system is broken. We’re just rearranging deck chairs on the Titanic. Also, I once saw a guy give morphine instead of methadone because the label was smudged. He cried for a week. But the hospital didn’t change anything. Just gave him a ‘wellness seminar’.
Love this post! In India, we have a lot of regional languages - so when we print labels, we add the drug name in English, Hindi, and sometimes Tamil. And we always write the purpose in big letters: ‘FOR SEIZURES’ or ‘FOR HIGH BP’. It’s not fancy, but it saves lives. Also, we teach this in pharmacy school from day one. No excuses.
Let’s not pretend this is about patient safety. It’s about liability. Hospitals use TML because the Joint Commission says so - not because they care. If you look at the real data, most LASA errors happen in outpatient settings where TML isn’t even enforced. The whole thing is performative. We’re creating a checklist culture. People check the box, then go back to rushing. And when someone dies? ‘Oh no, we followed protocol!’ - but they didn’t. They just ticked a box.
Hey, I just started working in a hospital pharmacy and I had no idea about this. I’m not trying to sound like a know-it-all, but… what if we just stopped using names that look alike? Like, why do we even need ‘hydroxyzine’ and ‘hydralazine’? Why not rename one? Is it really that hard? I mean, if you can name a drug ‘Lipitor’ or ‘Zoloft’, you can name one ‘Hydro-Sleep’ or ‘Hydro-Vas’. It’s not rocket science.
Also, I love that Johns Hopkins added purpose notes. That’s genius. If the script says ‘for anxiety’ next to hydroxyzine, and the bottle says ‘for hypertension’, you don’t even need to read the name. You just know it’s wrong. Why isn’t this mandatory everywhere?
You know what’s even more terrifying? The fact that most patients don’t even know what their meds are for. I had a guy come in asking for ‘the blue pill for my nerves’ - turned out he was supposed to be on hydroxyzine, but got hydralazine because the pharmacist didn’t ask what it was for. And the guy had been taking it for three weeks. No one checked. No one cared. We’re not just failing systems. We’re failing people. And we’re pretending it’s just a typo problem.