By 2025, Medicare Part D is saving millions of seniors hundreds of dollars a year on generic prescriptions - and it’s not just because drugs got cheaper. The real change? The rules changed. If you’re on Medicare and take generic meds, you’re likely paying less than you ever have before. But knowing how it works can mean the difference between saving $400 a year or still getting hit with surprise bills.
What Changed in 2025?
Before 2025, if you took multiple generic drugs, you could spend up to $8,000 out of pocket before your Part D plan kicked in to cover the rest. That’s not a typo. Eight thousand dollars. Many seniors skipped doses or split pills just to stretch their budgets. Now, thanks to the Inflation Reduction Act, your maximum out-of-pocket spending for all prescriptions - brand or generic - is capped at $2,000 per year. Once you hit that number, you pay $0 for the rest of the year. That’s a 75% drop in potential costs.How Much Do Generics Actually Cost Now?
Most generic drugs fall into the lowest tier on Part D formularies. In 2025, the typical copay for a 30-day supply of a preferred generic is around $10. Some plans charge as little as $5. If you’re on a low-income subsidy (Extra Help), you might pay $0 to $4.50. And here’s the kicker: you don’t have to wait until you hit the $2,000 cap to see savings. The 25% coinsurance you pay during the initial coverage phase is already lower than what most people paid before.For example, if you take three generic medications that cost $30 each per month, your annual out-of-pocket cost under the old system might have been $1,080 just for the drugs - not counting the deductible. Now, with the $2,000 cap, you’re paying that same $1,080, but you’re also getting closer to $0 for the rest of the year. And if you take more than five generics, you’ll likely hit the cap before the year ends.
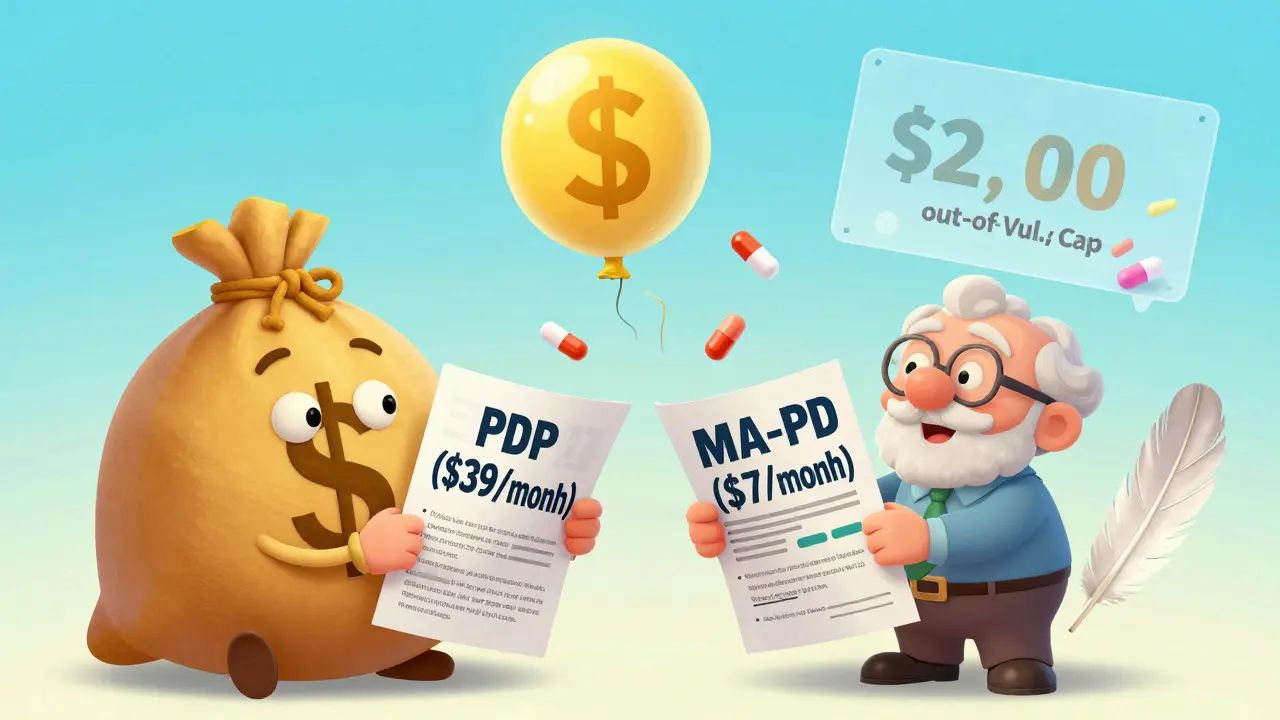
Part D Plans: PDP vs. MA-PD
There are two main ways to get Part D coverage: standalone Prescription Drug Plans (PDPs) or Medicare Advantage Prescription Drug plans (MA-PDs). Both cover generics the same way under federal rules, but the costs look very different.PDPs usually charge higher monthly premiums - around $39 on average. But your copays for generics are still $10 or less. MA-PDs, which bundle your Medicare Parts A, B, and D into one plan, have an average drug premium of just $7. That’s over five times cheaper. So if you’re comparing plans, don’t just look at copays. Add up the total: monthly premium + copays + deductible. Many people save more by switching from a PDP to an MA-PD, even if the copay is slightly higher.
What Counts Toward the ,000 Cap?
Not everything you pay counts. Your monthly premium doesn’t. But everything else does: deductibles, copays, coinsurance, and even what you pay at the pharmacy. Even manufacturer discounts - like those from drug companies under the Inflation Reduction Act - count toward your cap. That’s new. Before, those discounts didn’t help you reach the cap faster. Now, they do. That’s why some people hit $2,000 in just six months.Here’s how it works: if you pay $120 for a generic drug and the manufacturer gives you a $40 discount, your total out-of-pocket cost is $80. But $160 counts toward your cap - $120 you paid, plus $40 from the manufacturer. That’s a big deal if you’re on multiple high-cost generics.
Why Some People Still Pay More Than Expected
The system is simpler now, but it’s still confusing. A 2024 study found that 41% of Medicare beneficiaries didn’t understand how manufacturer discounts counted toward their $2,000 cap. Others didn’t realize their plan could switch their generic to a different version with a higher copay. That’s called therapeutic substitution. If your blood pressure pill changes from a $5 generic to a $15 one - even if it’s still technically a generic - your costs go up.Also, not all plans cover the same generics. One plan might list lisinopril as a preferred generic. Another might require you to try a different brand first. That’s called step therapy. About 27% of Part D plans use step therapy for at least 15 generic drug classes. So if you’re switching plans, check the formulary - not just the copay.
Who Saves the Most?
The biggest savings go to people who take multiple generic drugs. Someone on five or more generics can save over $600 a year. People on insulin or other expensive brand-name drugs also benefit, but the real win is for those on routine generics: blood pressure pills, statins, metformin, levothyroxine, and similar drugs. The average beneficiary taking mostly generics saves about $400 annually. That’s $33 a month - enough to cover a grocery trip or a monthly phone bill.Low-income beneficiaries on Extra Help save even more. They pay $0 deductible and $0 to $4.50 copays. They don’t have a coverage gap at all. That’s the most stable part of the system.
How to Find the Best Plan for Your Generics
The Medicare Plan Finder tool is your best friend. Go to medicare.gov and enter your exact medications, dosages, and pharmacy. The tool shows you exactly how much you’ll pay under each plan - including how quickly you’ll hit the $2,000 cap. Don’t guess. Use the tool. In 2024, a GAO report found that 32% of users needed help navigating it. Call 1-800-MEDICARE. Ask them to walk you through it.Check if your pharmacy is in-network. Some plans have preferred pharmacies that charge lower copays. CVS, Walgreens, and Walmart often offer $4 generic lists for Part D enrollees. That’s $4 for a 30-day supply - better than most plan copays.
What’s Coming Next?
In 2026, a new program will give plans a 10% subsidy to lower copays for certain high-cost generics - like those used for autoimmune or mental health conditions. That could bring more generics down to $5 or less. Also, biosimilars - generic versions of biologic drugs - are starting to appear in Part D formularies. These aren’t traditional generics, but they work the same way: lower cost, same effect. By 2028, they could cut costs for thousands.For now, the $2,000 cap is the biggest win. It’s not perfect. Some plans still restrict access. Some pharmacies still don’t explain how discounts work. But if you’re on generics, you’re paying less than ever. And that’s the bottom line.
Do generic drugs work as well as brand-name drugs under Medicare Part D?
Yes. Generic drugs are required by the FDA to have the same active ingredients, strength, dosage, and effectiveness as their brand-name versions. Medicare Part D plans cover generics because they’re proven to be just as safe and effective - and they save the program billions. The only difference is the price and the inactive ingredients (like fillers or dyes), which don’t affect how the drug works.
Does my monthly premium count toward the $2,000 out-of-pocket cap?
No. Your monthly premium does not count toward the $2,000 out-of-pocket cap. Only what you pay at the pharmacy - including deductibles, copays, and coinsurance - counts. Manufacturer discounts also count. But your premium is separate and doesn’t help you reach the cap faster.
Can my Part D plan switch my generic drug without telling me?
Yes, under certain conditions. Plans can substitute one generic for another if they’re considered therapeutically equivalent. This is called therapeutic interchange. While it’s legal, your plan must notify you in advance. If your copay jumps from $5 to $15 after the switch, you can appeal or switch plans during Open Enrollment.
How do I know if I qualify for Extra Help?
You may qualify if your income is below $21,870 for a single person or $29,580 for a couple in 2025, and your resources (savings, investments, property) are under $17,220 for a single person or $34,360 for a couple. You can apply through Social Security. If you get Medicaid, SNAP, or SSI, you’re automatically eligible. Extra Help means $0 deductible and $0-$4.50 copays for generics.
What if my generic drug isn’t covered by my Part D plan?
If your drug isn’t on the formulary, you can request an exception. Your doctor can submit a form explaining why you need that specific generic - maybe because others caused side effects. If denied, you can appeal. You can also switch plans during Open Enrollment (October 15 to December 7) to one that covers your medication.





One comment
Finally some real relief for seniors on meds. I’ve been watching my mom struggle for years and this change is life-changing.
i just found out my plan switched my blood pressure med to a different generic last month and my copay went from $5 to $15... no notice. how do i fight this??
Man, this system used to feel like a maze with no exit. Now? It’s like someone turned on the lights. I’ve been on three generics for ten years-metformin, lisinopril, atorvastatin-and last year I dropped $1,200. This year? I’m already halfway to the cap by June. That’s not just savings-that’s dignity.
And the manufacturer discounts counting? That’s the quiet hero here. I didn’t even know those were real money in the game until I checked my statement. Now I’m actually looking forward to refill day.
People say government doesn’t help. But when it does? It doesn’t whisper. It roars.
I’ve seen friends skip pills. I’ve seen grandmas split tablets with a knife. That’s not healthcare. That’s survival. And now? We’re not surviving-we’re living.
It’s not perfect. Some plans still play games. But the cap? That’s the anchor. Everything else is just noise.
And for those still confused? Go to medicare.gov. Type in your meds. Let the tool do the math. Don’t guess. Don’t hope. Calculate.
And if you’re on Extra Help? You’re already winning. Just don’t stop checking. Because the system changes. But you? You’ve got to stay sharp.
This isn’t politics. This is pills. This is breath. This is waking up without wondering if you can afford tomorrow.
They say change is slow. But sometimes? It hits like a thunderclap. And today? I’m grateful.
So let me get this straight-you pay $2000 a year, and then everything’s free? And the drug companies are paying part of that? Wow. I guess even capitalism can be convinced to share.
My aunt hit the cap in August. She cried when she told me. Not because she was sad. Because she could finally buy her cat’s insulin without choosing between groceries and vet bills.
It is imperative to note that the $2,000 out-of-pocket cap represents a monumental shift in federal healthcare policy. This is not merely a cost reduction-it is a restoration of human dignity for millions of elderly Americans who previously faced impossible trade-offs between pharmaceutical necessity and basic subsistence.
Furthermore, the inclusion of manufacturer discounts as qualifying expenditures toward the cap is a profoundly intelligent regulatory design. It incentivizes pharmaceutical innovation while simultaneously protecting vulnerable populations.
It is also noteworthy that Medicare Advantage Prescription Drug plans (MA-PDs) offer significantly lower monthly premiums than standalone PDPs, making them the optimal financial choice for the majority of beneficiaries.
However, one must remain vigilant regarding therapeutic substitution and formulary changes. These administrative maneuvers, while technically permissible, can undermine the very savings the policy intends to deliver.
Therefore, I strongly recommend that all beneficiaries utilize the Medicare Plan Finder tool annually-not merely during Open Enrollment, but as a continuous practice of financial stewardship.
The Inflation Reduction Act, despite political opposition, has delivered one of the most tangible, life-affirming outcomes of recent federal legislation.
Let us not take this for granted. Let us protect it. Let us expand it.
Oh great. So now the government is making drug companies pay for their own greed? What’s next? Will they start forcing billionaires to give back their yachts? This is socialism with a smiley face. They’re just making you think you’re getting a deal while they take your freedom away.
And don’t even get me started on how they’re counting manufacturer discounts. That’s just a trick to make the numbers look good. The real cost is still coming out of your taxes. You think these companies are doing this out of the goodness of their hearts? They’re just playing the game.
And why are we letting foreigners like India and Nigeria get in on this? Are we just handing out American healthcare like candy now?
My grandfather didn’t need this. He just took his pills and didn’t complain. Now everyone wants a handout.
Biggest thing I learned? Walmart’s $4 generics are still the real MVP. I switched from my PDP to an MA-PD with Walmart as preferred pharmacy and now I pay $4 for everything. Even my thyroid med. Zero deductible. No cap needed. Just $4.
And yeah, the manufacturer discounts count now? That’s wild. I didn’t even know I was getting them. Turns out my blood pressure pill’s maker gives me $30 off every time I refill. So I pay $10, but $40 counts toward the cap. That’s like getting paid to be sick.
Also-don’t sleep on Extra Help. If you’re even close to qualifying, APPLY. It’s not a handout. It’s a reset button.
And if your plan swaps your generic? Call them. Ask for the formulary change notice. If they didn’t send it? File a complaint. They’re supposed to.
This ain’t perfect. But it’s the best we’ve ever had. And if you’re not using the Plan Finder? You’re leaving money on the table. Like, hundreds. Every year.
So if I take five generics and hit the cap in July, do I still have to pay premiums? Or is that it?
Let me break this down for anyone still confused. You pay $2,000 total for ALL your meds in a year. After that? Free. No more bills. No more choosing between food and pills.
That includes copays. Deductibles. Even the discount the drug company gives you. That’s right-$40 discount from the maker? That counts as $40 toward your cap. So you pay $10, but $50 is gone from your out-of-pocket. That’s how you hit $2,000 in six months.
And if you’re on Extra Help? You’re basically playing on easy mode. $0 deductible. $0 to $4.50 per script. No cap needed. You’re already winning.
Don’t waste time guessing. Go to medicare.gov. Type in your exact meds. Pick your pharmacy. Watch the numbers change in real time. It’s like a video game where the reward is not dying broke.
And if your plan swaps your generic? You have rights. You can appeal. You can switch. You don’t have to take it.
This isn’t magic. It’s policy. And it works. Use it.
Wow. So now I don’t have to stress about my meds? That’s… nice. I guess.
Just checked my plan-my statin went from $10 to $4 at CVS. And the discount from the maker? It’s already counting. I’m gonna cry. Not because I’m sad. Because I finally feel safe.
Thank you to whoever made this happen. 🙏
As a dedicated advocate for equitable healthcare access, I must commend the structural reforms embedded within the Inflation Reduction Act’s implementation of Medicare Part D. The cap on out-of-pocket expenditures at $2,000 is not merely a fiscal adjustment-it is a moral imperative fulfilled. The inclusion of manufacturer discounts as qualifying expenditures toward this cap is a masterstroke of policy design, ensuring that pharmaceutical cost-reduction mechanisms directly benefit the patient rather than merely reducing insurer liability.
Furthermore, the distinction between standalone PDPs and MA-PDs reveals a critical insight: affordability is not determined solely by copay amounts, but by the aggregate cost of premiums, deductibles, and out-of-pocket spending. Many beneficiaries remain unaware that a plan with a slightly higher copay but a $7 monthly premium may yield greater annual savings than a $39 PDP with lower copays.
Therapeutic substitution, while legally permissible, remains an ethical gray zone. The absence of proactive notification to patients constitutes a systemic failure in patient-centered care. I urge all beneficiaries to request a copy of their formulary annually, and to document any unexpected changes in copay structure.
Extra Help remains the most underutilized benefit in the entire Medicare ecosystem. Individuals with incomes under $21,870 (single) or $29,580 (couple) are eligible-yet a significant portion remain unenrolled due to stigma or misinformation. This is not welfare. This is justice.
Finally, the impending introduction of biosimilars in 2028 may revolutionize access to biologic medications for autoimmune and oncology patients. This is not the end of reform-it is the beginning of a new era.
Let us not celebrate this as a gift. Let us defend it as a right.
My dad’s on four generics. He used to refill every month like clockwork-then he’d skip a week to make it last. Last year he told me he cried when his pharmacy told him his total out-of-pocket was $312. Not $3,120. $312. He didn’t believe them. He checked his statement three times.
He’s not rich. He’s not loud. He just takes his pills. Now he doesn’t have to choose.
That’s the real win here.