Sore Throat Cause Quiz
Answer the following questions to determine whether your sore throat is likely caused by allergies or an infection.
1. Did your sore throat start immediately after being exposed to something?
2. Do you have itchy eyes, sneezing, or a runny nose along with the sore throat?
3. Are you experiencing a fever?
4. Is your throat pain accompanied by swollen lymph nodes or body aches?
5. Do you have thick yellow or green mucus?
Ever felt a tickle in your throat that just won’t quit, only to discover it’s linked to your seasonal sniffles? That nagging soreness isn’t always a cold - it can be your body reacting to allergens. Below you’ll learn why allergies often bring a sore throat, how to tell the difference from an infection, and practical steps to feel better fast.
Quick Takeaways
- Allergens trigger histamine release, leading to swelling and post‑nasal drip that irritates the throat.
- Common culprits include pollen, dust mites, pet dander, and mold spores.
- Allergy‑related sore throats are usually dry, itchy, and worse after exposure, while infections bring fever and pus‑filled tonsils.
- Antihistamines, nasal rinses, and humidified air can clear the throat in hours.
- See a doctor if pain lasts more than a week, is severe, or is accompanied by difficulty breathing.
Why Allergies Can Scratch Your Throat
When an Allergy is an immune system overreaction to typically harmless substances such as pollen, dust, or animal dander hits your nose or eyes, the body releases a flood of Histamine a chemical messenger that expands blood vessels and increases mucus production. This extra mucus drips down the back of the throat - a process called Postnasal drip the steady flow of mucus from the nasal passages to the throat. As the mucus sits, it carries irritants and enzymes that scrape the delicate lining, creating that raw, sore feeling.
At the same time, histamine makes the throat’s blood vessels swell, a condition known as Allergic rhinitis inflammation of the nasal lining caused by an allergic response. Swollen tissue produces even more mucus, turning the cycle into a self‑reinforcing loop.
Allergens Most Likely to Trigger a Sore Throat
- Pollen - tree, grass, and weed pollen peak in spring and early fall; they travel far on the wind and settle on indoor surfaces.
- Dust mites - microscopic creatures that love the humidity in bedding, carpets, and upholstered furniture.
- Pet dander - tiny skin flakes from cats, dogs, and even birds; they cling to clothing and linger on furniture.
- Mold spores - thrive in damp basements, bathrooms, and any area with poor ventilation.
- Food allergens - peanuts, shellfish, or dairy can cause oral allergy syndrome, which sometimes spreads to the throat.
Notice a pattern? Most of these allergens are airborne or settle on surfaces we touch daily. Reducing exposure is the first line of defense.

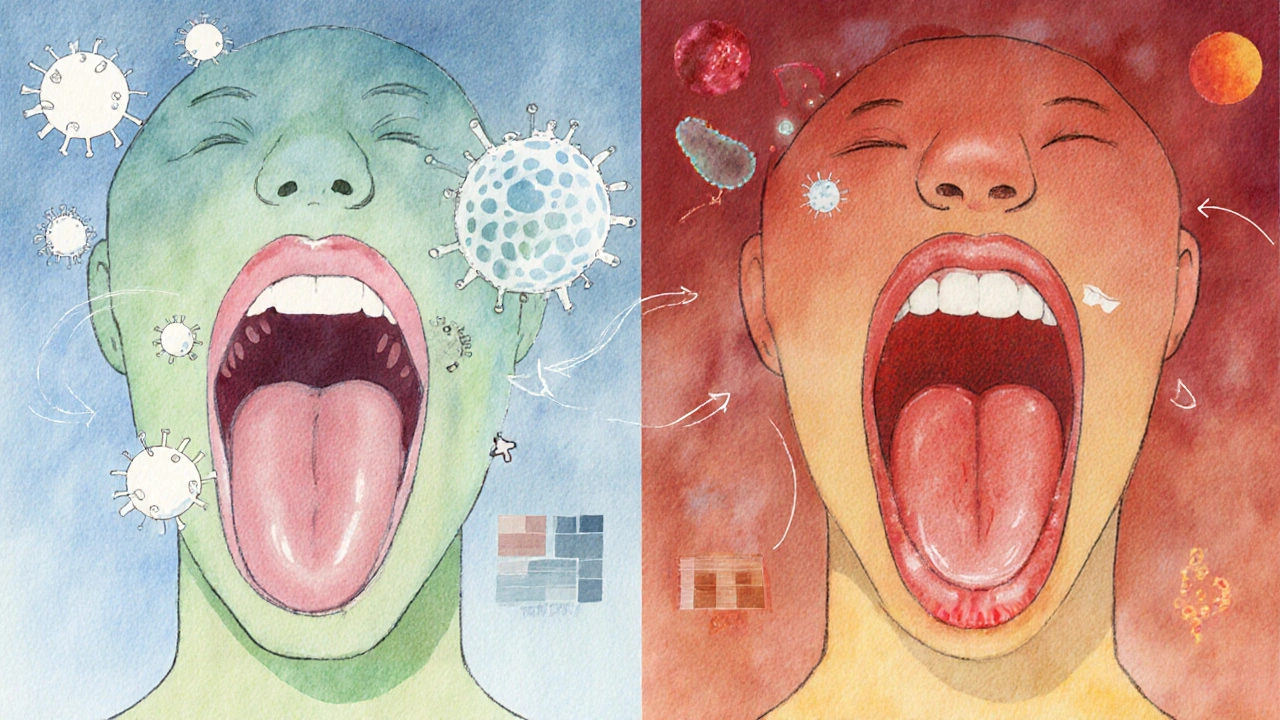
Allergy‑Related Sore Throat vs. Infection: Spot the Difference
| Feature | Allergic Sore Throat | Infectious Sore Throat |
|---|---|---|
| Onset | Immediate after exposure to trigger | Gradual, often after a cold |
| Pain level | Mild to moderate, often itchy | Moderate to severe, burning |
| Fever | Usually none | Common (often 100‑102°F) |
| Mucus | Clear, thin, excess post‑nasal drip | Yellow/green, thick, may be absent |
| Other symptoms | Watery eyes, sneezing, itchy nose | Body aches, swollen lymph nodes |
When you can line up these clues, you’ll know whether a quick antihistamine will help or if a doctor’s prescription is needed.
Fast‑Acting Ways to Calm an Allergy‑Induced Throat
- Take an antihistamine. Over‑the‑counter options like cetirizine or loratadine block histamine receptors, reducing swelling and mucus production. Start with the recommended dose; most people feel relief within 30‑60 minutes.
- Rinse your nasal passages. A saline spray or neti pot flushes out allergens and excess mucus, cutting the post‑nasal drip at its source. Use distilled or boiled‑then‑cooled water to avoid infections.
- Stay hydrated. Warm teas (ginger, chamomile) thin the mucus, making it easier to swallow rather than cling to your throat.
- Humidify the air. Dry indoor air amplifies irritation. A small humidifier set to 40‑50% humidity keeps the throat lining supple.
- Use throat lozenges with menthol or honey. These coat the throat temporarily, soothing the itch while the other measures work.
These steps target the root cause - histamine and mucus - rather than just masking pain.
When to Call a Healthcare Professional
Most allergy‑related throat soreness clears up within a week. However, seek medical advice if you notice any of the following:
- Severe pain that prevents swallowing or talking
- Fever above 101°F (38.3°C)
- White patches on the tonsils or a rash that spreads
- Shortness of breath, wheezing, or swelling of the lips/tongue (possible anaphylaxis)
- Pain lasting longer than 10‑14 days despite treatment
In such cases, a doctor may prescribe a stronger antihistamine, a nasal corticosteroid spray, or an oral steroid burst to break the inflammation cycle.
Long‑Term Prevention: Keep Allergens at Bay
Prevention is the most sustainable fix. Here are proven habits that lower the odds of an allergy‑driven sore throat:
- Allergy‑proof your bedroom: Use allergen‑impermeable pillowcases, wash bedding weekly in hot water (130°F), and keep humidity below 50%.
- Seal windows during high pollen days and run an air purifier with a HEPA filter in the living spaces you use most.
- Vacuum with a HEPA‑rated vacuum twice a week; dust mites and dander love carpet fibers.
- Shower before bed to rinse pollen off your hair and skin after a day outdoors.
- Consider allergy immunotherapy (shots or sublingual tablets) if you’re constantly battling symptoms. It reshapes the immune response over months.
Combining these habits with the quick‑relief steps above makes it far less likely that a simple sneeze will turn into a painful throat.
Frequently Asked Questions
Can a sore throat be the only sign of an allergy?
Yes. Some people experience “silent” allergies where the throat feels raw, but the classic runny‑nose or itchy eyes are minimal. In these cases, post‑nasal drip is the main culprit.
Are antihistamines safe for children?
Most second‑generation antihistamines (like cetirizine) are approved for kids over 2 years, but dosing is weight‑based. Always check the label and consult a pediatrician.
Why does my throat feel worse at night?
Lying down allows mucus to pool in the back of the throat, increasing irritation. Using an extra pillow to elevate your head and a humidifier can lessen nighttime soreness.
Can oral allergy syndrome cause throat pain?
Yes. Foods that share protein structures with pollen (like apples for birch pollen) can trigger itching and mild swelling in the mouth and throat, known as oral allergy syndrome.
When should I consider allergy shots?
If you need daily antihistamines, have frequent sinus infections, or suffer from asthma triggered by allergens, immunotherapy can reduce long‑term sensitivity. A specialist can run skin‑prick or blood tests to design a personalized plan.





One comment
Look, I get that the article ties post‑nasal drip to that scratchy feeling, but anyone who’s ever caught a cold knows the line isn’t that clear. Histamine isn’t the only irritant; viral particles can trigger similar mucus production. Plus, many of us in India still rely on home remedies that don’t involve antihistamines at all. So while the checklist is handy, it’s not a universal cure‑all. Think of it as a starting point, not a final verdict.
Oh sure, because popping a couple of antihistamines is gonna magically turn your throat into a silk scarf. 🎭 The article totally ignores the fact that some people get a full‑blown infection even after the first sneeze. And let’s not forget that “humidify the air” advice is basically telling you to buy a pricey gadget you’ll forget to clean. Bottom line: the guide is a decent cheat sheet, but it’s as bland as unsalted popcorn.
While the piece correctly outlines the role of histamine, it could benefit from a clearer distinction between allergic rhinitis and viral pharyngitis. Adding a quick reference to the typical duration of each condition would enhance its utility. Also, an emoji might lighten the tone, but the content remains solid. 👍
TL;DR: allergies = histamine → mucus → throat irritation; infections = virus/bacteria → fever + pus. Use antihistamines for the former, see a doc for the latter. Keep it concise.
Honestly, the advice on nasal rinses is top‑notch, but you could sprinkle a bit more sarcasm about the “just drink water” cliché. Still, the step‑by‑step list is practical, and the quiz adds some interactivity. Keep the friendly vibe, but maybe warn readers about over‑doing neti pots.
The article presents a well‑structured overview of allergy‑induced sore throats, yet it could benefit from a more formal citation of clinical guidelines. Incorporating references to the American Academy of Otolaryngology would bolster credibility. Nonetheless, the practical tips on humidification and lozenges are valuable for lay readers.
Great quick‑take summary.
Man, this article kinda hits the nail. Real talk – I tried the saline spray and felt better fast. But watch out for using tap water, can get you sick. Also, dnt forget to clean yo neti pot. Overall good tips, tho.
Behold, the ultimate saga of sneezes and sore throats! This piece drapes itself in jargon like a velvet cape, yet somehow manages to keep the drama alive. From pollen‑provoked post‑nasal drip to the dreaded yellow mucus, every twist is narrated with theatrical flair. The checklist feels like a heroic quest, and the remedies are the magical potions you’d expect in a fantasy epic. If you’re looking for a mundane medical briefing, you won’t find it here – you’ll find a story worth a standing ovation.
The guide is solid, but a few grammatical tweaks would improve readability. For instance, “post‑nasal drip” should be hyphenated consistently. Also, adding bullet points for the “when to see a doctor” section could help readers skim faster. Overall, the content is helpful and balanced.
One must question the originality of this composition; it rehashes well‑trod advice without offering novel insight. The reliance on generic internet sources renders the piece pedestrian at best.
Wow!!! This article really dives deep into the whole allergy‑induced sore throat thing!!! 😲 First, the explanation of histamine release is spot‑on, and it really helps you understand why that tickle happens. Second, the list of allergens – pollen, dust mites, pet dander, mold – is exhaustive, which is great for anyone trying to pinpoint the culprit. Third, the quiz format is interactive and keeps readers engaged, making the information stick. Fourth, the practical steps – antihistamines, nasal rinses, humidifiers – are described in a way that’s easy to follow. Fifth, the emphasis on when to see a doctor is crucial; you don’t want to ignore red‑flag symptoms. Sixth, the long‑term prevention tips, like using HEPA filters and washing bedding, are often overlooked in other articles. Seventh, I love that the piece mentions oral allergy syndrome, which many people miss entirely. Eighth, the tone remains conversational yet informative, striking a nice balance. Ninth, the formatting with bullet points and tables aids readability. Tenth, the inclusion of FAQs addresses common concerns directly. Eleventh, the advice on nighttime care – extra pillow, humidifier – is practical for anyone suffering at night. Twelfth, the suggestion of allergy immunotherapy offers hope for long‑term relief. Thirteenth, the article avoids overly medical jargon, making it accessible. Fourteenth, the consistent use of bold for key terms draws attention to important concepts. Fifteenth, the overall structure flows logically from cause to treatment to prevention. In short, this piece is thorough, user‑friendly, and packed with actionable advice! 😃
Reading this gave me confidence that a simple antihistamine and a good humidifier can really turn the tide on that annoying throat tickle. Keep spreading the word!
Honestly, the article just scratches the surface and fails to address the deeper issues of over‑reliance on medication.
As someone who values our nation's health, I must stress that ignoring allergens is a betrayal of our collective well‑being. The guide’s recommendations are solid, but we need stronger public policies to reduce pollen exposure in our cities. Only then will our throats-and our pride-truly be protected.